Interesting Statistics Regarding Acid Reflux
 Acid Reflux is common among all ages and populations in the world
Acid Reflux is common among all ages and populations in the world- More than 60 million Americans experience heartburn at least once a month.1
- 15 million Americans experience heartburn symptoms each day.1
- Gastroesophageal reflux disease (GERD) or chronic acid reflux is a common condition affecting around 20% of the U.S. population.
- Acid Reflux costs our medical system $12 billion dollars per year.2
- Globally more than $7 billion dollars is spent on antacids each year.3
Definition of Acid Reflux / Heartburn / GERD / Barrett’s Esophagus
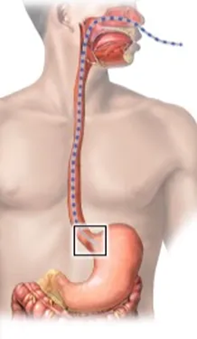
Acid Reflux is a condition in which acidic gastric fluid flows backward from the stomach into the esophagus, resulting in heartburn
Heartburn is a form of indigestion felt as a burning sensation in the chest, caused by acid regurgitation into the esophagus.
GERD is short for gastroesophageal reflux disease. It’s a condition in which acidic gastric fluid flows backward into the esophagus, resulting in heartburn.
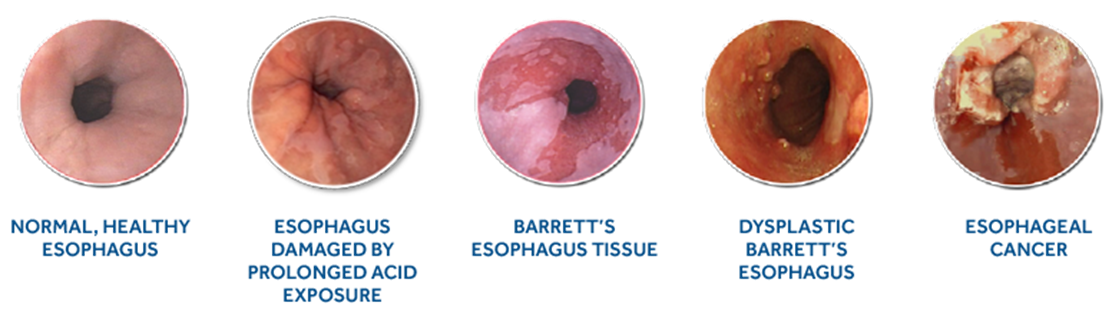
Barrett’s Esophagus is a condition in which the flat pink lining of the esophagus, (the swallowing tube that connects the mouth to the stomach) becomes damaged due to chronic exposure to acid from the stomach. The lining becomes thickened and red. This triggers a change in the cells of the lining that can then lead to the formation of Barrett’s esophagus.
These definitions can be confusing for patients. To try and clear things up, if you have Acid Reflux, you could experience Heartburn. GERD is the formal diagnosis of chronic Acid Reflux. Barrett’s Esophagus is a condition that occurs after years of untreated chronic Acid Reflux.
Causes of Acid Reflux / GERD
Doctors still debate about the primary cause of Acid Reflux. Some of the most common causes include the following:4
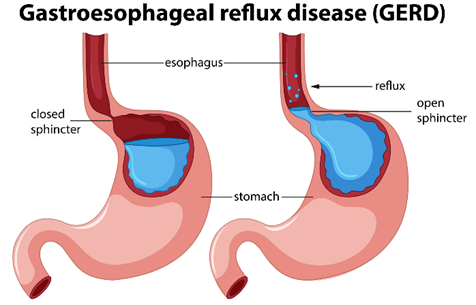 Certain foods and drinks – such as coffee, tomatoes, alcohol, chocolate and fatty or spicy foods causing the sphincter muscle to relax at the base of the esophagus.
Certain foods and drinks – such as coffee, tomatoes, alcohol, chocolate and fatty or spicy foods causing the sphincter muscle to relax at the base of the esophagus.- Eating a heavy meal and lying on your back or bending over at the waist.
- Snacking close to bedtime or lying down right after a meal.
- Taking aspirin or ibuprofen, some muscle relaxers, or certain blood pressure medications.
- Being overweight.
- Smoking.
- Pregnancy.
- Stress, anxiety and depression.
- Delayed stomach emptying.
- An increase in some types of hormones, such as progesterone and estrogen.
- A hiatal hernia – when part of your stomach moves up into your chest.
- A stomach ulcer.
- A bacterial infection in your stomach – such as Helicobacter pylori infection.
- An overproduction of acid due to not digesting food well.
- Lack of digestive enzymes.
Symptoms of Acid Reflux
The following are the most common symptoms of Acid Reflux / GERD. However, everyone may experience symptoms differently. Symptoms may include:
- A burning sensation in your chest (heartburn), usually after eating, which might be worse at night or while lying down.
- Regurgitation (when stomach contents back up into the mouth).
- Upper abdominal or chest pain.
- Trouble swallowing (dysphagia).
- Sensation of a lump in your throat.
- A sour taste in the mouth.
- Nausea.
- Burping.
- Bloating.
- Dry cough or throat clearing repeatedly.
- Sore throat, hoarseness, or laryngitis.
- Shortness of breath.
The symptoms of Acid Reflux may resemble other medical conditions or problems such as gallstones, stomach ulcers, heart attack, and esophageal cancer. This is why it’s always important to consult a doctor for a proper diagnosis
How Chronic Acid Reflux (GERD) is Diagnosed
 Your health care provider might be able to diagnose GERD based on a history of your signs and symptoms and a physical examination. To confirm a diagnosis of GERD, or to check for complications, your doctor might recommend:5
Your health care provider might be able to diagnose GERD based on a history of your signs and symptoms and a physical examination. To confirm a diagnosis of GERD, or to check for complications, your doctor might recommend:5
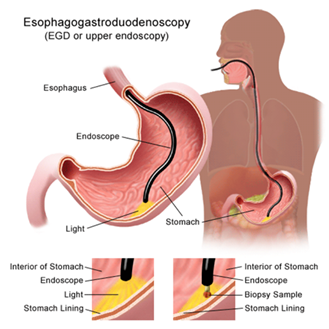
- Upper Endoscopy. Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat. The endoscope helps your provider see inside your esophagus and stomach. Test results may not show problems when reflux is present, but an endoscopy may detect inflammation of the esophagus (esophagitis) or other injury to the esophagus, and other complications.
- An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett esophagus. In some instances, if a narrowing is seen in the esophagus, it can be stretched or dilated during this procedure. This is done to improve trouble swallowing (dysphagia).
- Ambulatory Acid (pH) Probe Test. A monitor is placed in your esophagus to identify whether acid is being refluxed into the esophagus from the stomach and to measure how much acid is being refluxed. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder.
- The monitor might be a thin, flexible tube (catheter) that's threaded through your nose into your esophagus. Or it might be a clip that's placed in your esophagus during an endoscopy. The clip passes into your stool after about two days.
 X-ray of the Upper Digestive System. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing.
X-ray of the Upper Digestive System. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing.
- You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
- Esophageal Manometry. This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus. This is typically done in people who have trouble swallowing.
- Trans Nasal Esophagoscopy This test is done to look for any damage in your esophagus. A thin, flexible tube with a video camera is put through your nose and moved down your throat into the esophagus. The camera sends pictures to a video screen.
Types of Acid Reflux
There are four types of acid reflux mild, moderate, severe and the type that can lead to esophageal cancer. There is also a diagnosis called Silent Reflux that is important to mention.
- Mild Acid Reflux / GERD6 this is the first stage of gastroesophageal reflux disease. If you have GERD, it's likely that you have this kind. With mild acid reflux, the lower part of your esophagus will be mildly inflamed. If you have stage 1 acid reflux, you might experience:
- Heartburn
- Pain in your chest
- Feel a lump in the back of your throat
- Regurgitate food and liquid
- Moderate Acid Reflux / GERD about a third of people with acid reflux fall into stage 2. The main difference between mild and moderate acid reflux is that your symptoms will happen multiple times a week, resulting in more irritation and inflammation in your esophagus. Left untreated, it can affect your day-to-day activities. You’ll likely need to take acid-suppressive medicines daily.
- Severe Acid Reflux / GERD if you have stage three acid reflux, you’re probably already taking prescription medication and dealing with extreme symptoms every day. It’s likely that you’ll have erosive esophageal inflammation. About 15% of people with acid reflux fall into this third stage. In this stage you are probably experiencing:
- Heartburn
- Regurgitating food and liquid
- Sore throat
- Hoarseness
- Coughing that doesn’t get better
- Esophageal Cancer After many years of untreated stage three acid reflux, you could develop precancerous lesions (i.e. Barrett’s esophagus) and/or esophageal cancer. Around 10% of people who have GERD for a long period of time make it to this type of acid reflux. Barrett’s Esophagus is a precancerous condition that over time, can turn into cancer if it remains untreated. If you have stage four reflux, you might have:
- Heartburn
- Regurgitating food and liquid
- Sore throat
- Hoarseness
- Coughing that doesn’t get better
- Food getting stuck in your esophagus while you eat
- Silent Reflux also known as laryngopharyngeal reflux (LPR), is a condition in which stomach acid flows back up the esophagus (swallowing tube) into the larynx (voice box) and throat. LPR is called silent reflux because it often does not cause any symptoms in the chest. Patients diagnosed with Silent Reflux are found to have inflammation in the esophagus but don’t feel any symptoms associated with it.
Traditional Medical Treatment for Acid Reflux
Your doctor is likely to recommend that you first try lifestyle changes and nonprescription medications.
Lifestyle Changes Include:
- Maintain a healthy weight. Excess pounds put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Stop smoking Smoking decreases the lower esophageal sphincter's ability to function properly
- Elevate the head of your bed If you regularly experience heartburn while trying to sleep, place wood or cement blocks under the feet at the head-end of your bed. Raise the head-end by 6 to 9 inches. If you can't elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows is typically not effective.
- Start on your left side. When you go to bed, start by lying on your left side to help make it less likely that you will have reflux. The stomach drains best when you are on your left side.
- Don't lie down after a meal. Wait at least three hours after eating before lying down or going to bed.
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Avoid foods and drinks that trigger reflux.Common triggers include alcohol, chocolate, caffeine, fatty foods or peppermint.
- Avoid tight-fitting clothingClothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
Nonprescription Medications Include:
 Antacids neutralize stomach acid Antacids containing calcium carbonate, such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won't heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.
Antacids neutralize stomach acid Antacids containing calcium carbonate, such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won't heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.- Medications to reduce acid production. These medications — known as histamine (H-2) blockers — include cimetidine (Tagamet HB), famotidine (Pepcid AC) and ranitidine (Zantac). H-2 blockers don't act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Medications that block acid production and heal the esophagus. These medications — known as proton pump inhibitors (PPI’s) — are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription PPI’s include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
If you start taking a nonprescription medication for GERD, be sure to inform your doctor. You should know that taking these medicines long-term do have side effects. It even states on the package that the medicine is to be taken on a short-term basis. Most patients who self-diagnose and put themselves on these over-the-counter medicines tend to stay on them long-term without being worked up by a Gastroenterologist; I strongly discourage this. If you find yourself needing to be on these medicines long-term, please see a Gastroenterologist to have a formal work-up right away.
If lifestyle changes and over-the-counter medicines are not cutting it, your doctor may suggest prescription strength treatments.
Prescription-Strength Treatments for GERD Include:
- Prescription-strength H-2 blockers. These include prescription-strength famotidine and nizatidine. Side effects from these medications are generally mild and well tolerated.
- Prescription-strength proton pump inhibitors (PPI’s). These include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant). Although generally well tolerated, these medications might cause diarrhea, headaches, nausea, or in rare instances, low vitamin B-12 or magnesium levels. There are also other potential long-term adverse side effects with taking the PPI’s that must be taken into consideration. By the time patients come to my office for a consultation, many of them have already been on at least one if not all three of these PPI’s and yet they are still having symptoms despite these treatments.
- Medications that block acid production and heal the esophagus. These medications — known as proton pump inhibitors (PPI’s) — are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription PPI’s include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
Depending on how bad the inflammation is in your esophagus or what organ structure changes are found during endoscopy (ex. Hiatal Hernia), your doctor may suggest other procedures or surgery.
Surgery and Other Procedures Include:
- Fundoplication The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure.
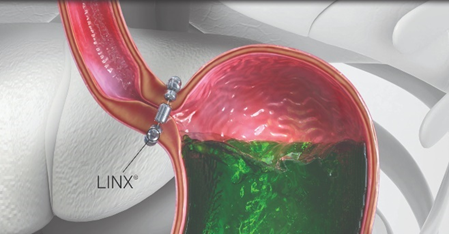 LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.
LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.- Transoral incisionless fundoplication (TIF). This non-surgical procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. TIF is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, TIF alone is not an option. However, TIF may be possible if it is combined with laparoscopic hiatal hernia repair.
Because obesity can be a risk factor for GERD, your health care provider could suggest weight-loss surgery as an option for treatment.
Complications of Acid Reflux
If you brush off Acid Reflux symptoms, more than likely it will progress into GERD and that can lead to other more serious health issues. Over time, stomach acid may damage your esophagus, teeth, and more. These complications can include:7
1. Damage to Your Esophagus
When the acid flows back up, it enters the esophagus, the tube that connects your mouth to your stomach. This can set the stage for:
- Esophagitis Stomach acid irritates the lining of the esophagus, causing it to swell. This inflammation is called esophagitis, which can lead to pain in the esophagus and/or painful swallowing.
- Esophageal ulcers: GERD is the top cause of ulcers, or sores in the lining of the esophagus. Symptoms include painful swallowing, pain in the esophagus, nausea, and chest pain.
- Esophageal stricture: Over time, the damage caused by stomach acid can scar the lining of the esophagus. When this scar tissue builds up, it makes the esophagus narrow. These narrow spots, called strictures, make it hard to swallow food and drinks, which can lead to weight loss and dehydration. Strictures are treated with a procedure that gently stretches your esophagus. On rare occasions it may require surgery.
- Esophageal stricture: Over time, the damage caused by stomach acid can scar the lining of the esophagus. When this scar tissue builds up, it makes the esophagus narrow. These narrow spots, called strictures, make it hard to swallow food and drinks, which can lead to weight loss and dehydration. Strictures are treated with a procedure that gently stretches your esophagus. On rare occasions it may require surgery.
- Barrett’s esophagus: About 5% to 10% of people with GERD develop this condition, where stomach acid causes precancerous changes in cells. The good news is that less than 1% of people with Barrett’s esophagus will get esophageal cancer.
2. Increased Risk of Esophagus Cancer
Having GERD slightly raises your odds of getting this type of cancer. Having Barrett’s esophagus can also make esophagus cancer more likely, especially if there’s a history of the condition in your family.
Symptoms of this type of cancer, such as troubling swallowing and chest pain, don’t appear until the disease reaches a later stage. That’s when it becomes harder to treat and at times it may be too late.
3. Tooth Decay
Heartburn can also take a toll on your smile. Stomach acid can wear down enamel, your teeth’s hard outer layer. This can weaken teeth and lead to cavities.
What Traditional Medicine is Not Telling You About Acid Reflux
The information I am about to share with you was not taught to me during any of my medical training. What medical school, internship, internal medicine residency, and my Gastroenterology fellowship taught me was how to diagnose symptoms, prescribe medicines and do amazing colonoscopies and upper endoscopies. What it didn’t teach was the true reason why people are having symptoms to begin with. And the idea that Acid Reflux / GERD can only be controlled with medicine, surgery or procedures is disconcerting.
All the items listed above under the causes of Acid Reflux are true, but the one cause that does not get addressed by traditional medicine is the overproduction of acid due to a lack of digestive enzymes being produced in the stomach.
There are two main reasons we are not producing enough digestive enzymes.
- As we age our enzyme production declines. We aren’t making all those great enzymes anymore to help us break down our food. This is why we start seeing patients in our office in their 40’s, 50’s and 60’s suddenly having issues with food. Patients will tell me all the time, they have never had a problem with food and now reflux, heartburn, out of the blue. To me, this is no longer a mystery.
- If we do not eat a nutritious well-balanced diet, we are not giving the body what it needs to produce a healthy number of digestive enzymes. I think we can all agree the Standard American Diet (SAD) leaves a lot to be desired. This is why we are seeing younger and younger patients in our office with the same digestive issues their parents and grandparents are experiencing. This is a generation of kids that have grown up on fast food, processed foods, fancy coffees, and energy drinks.
Taking both issues into consideration, if we don’t produce enough enzymes in our stomach when we eat, our food sits in our stomach too long causing more acid to be produced. It is this overproduction of acid that causes problems.
Traditional medicine will tell you that to fix your Acid Reflux you need to take a medicine that reduces or eliminates the acid being produced so you don’t have the symptoms. The problem is your stomach makes acid for reason, you need it to digest food properly, especially proteins. When you take acid reducing medicine, you’re not making acid or enzymes so imagine how much digestion is taking place in your stomach – not much!
 Take acid reducers long-term and this becomes a problem; one that I don’t believe traditional medicine really understands well enough to take seriously. I think most doctors feel their hands are tied because there are not many options for treating Acid Reflux. I think there is a reason for that too; there is a lot of money being made from acid reducing medicines today and that number is set to almost double over the course of the next 10 years.
Take acid reducers long-term and this becomes a problem; one that I don’t believe traditional medicine really understands well enough to take seriously. I think most doctors feel their hands are tied because there are not many options for treating Acid Reflux. I think there is a reason for that too; there is a lot of money being made from acid reducing medicines today and that number is set to almost double over the course of the next 10 years.
In addition, the current alternative therapies to treat GERD that are widely known in traditional medicine consist of the use of ginger, chamomile, and slippery elm. None of which have been proven through scientific studies to treat GERD or reverse damage to the esophagus; therefore, most traditionally trained doctors would not even consider them.
Although there is a place for traditional medicines in the treatment of Acid Reflux / GERD, it does not have to be a long-term strategy
Why It’s Important to Digest Your Food Properly
When you eat food, it goes into your stomach as a solid. Obviously, we chew it, but we don’t chew it into a liquid. Your body cannot use food in a solid form, it must be broken down into a liquid for your body to benefit from it. This means when you eat, your body is supposed to go to work for you – making enzymes and acid. There is a different enzyme produced to digest all different types of foods:
- Amylase & Diastase - break down starch into sugars / glucose.
- Protease- breaks down protein into amino acids.
- Lipase- breaks down fat into fatty acids.
- Invertase - breaks sugar down into glucose and fructose.
- Lactase - breaks down sugar found in dairy products.
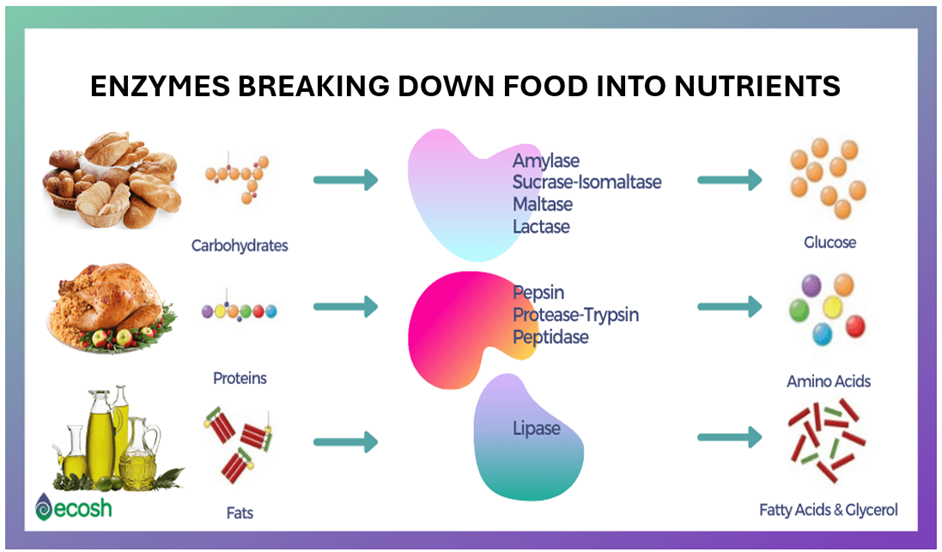
The acid that gets produced in the stomach helps to digest protein in addition to killing off germs, viruses or bugs found on our food. Our food is not sterile, so the acid helps to protect us from all the items we consume that the body shouldn’t be exposed to. Producing the appropriate amount of enzymes and acid is a crucial step in the digestive process. For your food to be absorbed and assimilated into the body the food must be broken down properly. If you are lacking enzymes or acid your food will sit around too long in the stomach causing lots of digestive issues but in addition to that you will not be able to benefit from the food itself.
Imagine this – even if you are eating the healthiest diet in the world, if your body is not breaking it down properly, you are not benefiting from what you are eating. This can cause you to be tired, have low energy, have a foggy brain, etc. Anyone out there experiencing any of these symptoms?
In addition, if you are not getting vitamins and minerals from the food you are eating, the body is very smart. It knows you need vitamins and minerals to function and so guess what it does, it starts to rob from itself. And the first place it goes is the bone and the muscle because that is where we have the most vitamins and minerals stored up.
Digesting your food properly is the first step to not only eliminating digestive issues but getting you off of over-the-counter and prescription meds while at the same time giving you your life back.
Long-Term Effects of Over-the-Counter Meds
There was a study released in 20218 that linked long-term use of PPI’s to damaging side-effects in the following areas of the body respiratory, kidney, liver, skeletal, central nervous system, cardiovascular, gastrointestinal, infections and blood deficiencies. Now that you understand the importance of enzymes and acid, you understand 4 key things:
- The reason you were probably having issues with Acid Reflux in the first place was due to a lack of enzymes.
- Taking PPI medicine cuts your acid production completely. You need some acid to digest protein in the food you are eating.
- When your body is not making enough enzymes or acid you can’t digest your food properly therefore benefit from what you are eating.
- When your body can’t get vitamins and minerals from food it starts to rob from itself.
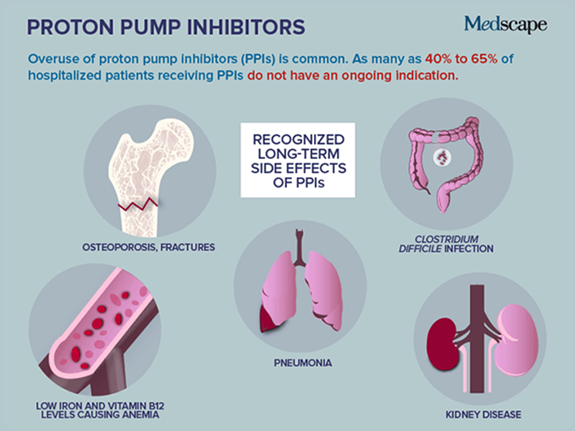 Is there any wonder why years and years of not absorbing vitamins and minerals leads to bone loss, muscle spasms, blood deficiencies, and issues with various systems of the body. Without vitamins and minerals your body cannot make healthy red blood cells. Healthy red blood cells make healthy tissue, which makes healthy organs, which makes a healthy body. It’s all connected and, in this case, not in a good way.
Is there any wonder why years and years of not absorbing vitamins and minerals leads to bone loss, muscle spasms, blood deficiencies, and issues with various systems of the body. Without vitamins and minerals your body cannot make healthy red blood cells. Healthy red blood cells make healthy tissue, which makes healthy organs, which makes a healthy body. It’s all connected and, in this case, not in a good way.
Over-the-counter and prescription medicines for Acid Reflux are not fixing the issue, they are a band-aid for it. And in the end, they are truly doing your body a disservice. If you truly want to be healthy, you must stop putting a band aid on the problem and start fixing it.
A Different Approach to Acid Reflux / GERD
In 2007, I approached my wife and Office Manager Tina and told her how frustrated I was with medicine. I was running all the tests, doing all the procedures, and prescribing all the medicines and could not figure out why my patients were still hurting. That frustration led us on a two-year journey to learn what my medical degree did not teach me about the body and how it works, in addition to what is happening in the medical industry, pharmaceutical industry and food industry to cause so many health problems in our society.
After we learned what we did, we felt obligated to share this with our patients and we’ve been doing so since 2010. Tina was so passionate about what we learned, she went back to school and received her Certificate in Holistic Nutrition so she could help me deliver this message to as many people as we possibly could. Since we started on this journey, we have helped tens of thousands of patients and wellness clients eliminate their symptoms naturally, helping their bodies work again like they were meant to work. And the best part of it all, is it’s not as hard as you may think to turn it all around, no matter how long you’ve been suffering or how old you are. If you are willing to put in the time, effort and invest in yourself, you can have your life back too.
As I mentioned above, there is a place for traditional medicine when treating Acid Reflux / GERD especially if you were found to have inflammation in the stomach or esophagus due to the issues. Anytime inflammation is found in a patient, I put them on PPI medicine. However, my goal is to get them off that medicine as soon as possible. We do that by testing them for food sensitivities, nutrient deficiencies and then using two key supplements.
Details on this approach are as follows:
 A Cellular Level Food Sensitivity Test Anyone struggling with Acid Reflux / GERD or Barrett’s Esophagus absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
A Cellular Level Food Sensitivity Test Anyone struggling with Acid Reflux / GERD or Barrett’s Esophagus absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
- Traditional allergists run skin and blood tests to determine food allergies. This food sensitivity test goes a level deeper to study the cellular level of the body, the difference between a food allergy and a food sensitivity.
 Micronutrient Test If you have been on a PPI medicine for a while, this test will test your blood for nutrient deficiencies at the cellular level. This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
Micronutrient Test If you have been on a PPI medicine for a while, this test will test your blood for nutrient deficiencies at the cellular level. This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
- This test is the ultimate guide to what foods and supplements you should and shouldn’t be consuming to offset your deficiencies. This test will give you the answer to why you are tired and have low energy. It is your chance to find out if all those supplements you are taking are necessary. Once you know what your cells really need, it becomes clear on how to replenish them.
- Digestive Enzymes As a recap, digestive enzymes help break down our food into smaller, more absorbable units. Your body cannot absorb the food you eat as is, it can only absorb nutrients. Therefore, for your body to benefit from what you eat, proteins need to be broken down into amino acids; fats need to be broken down into fatty acids and cholesterol; and carbohydrates need to be broken down into simple sugars. You rely on digestive enzymes to break down what you eat. One of the main reasons why we begin to suffer from Acid Reflux and Heartburn is because we are lacking digestive enzymes, and our food sits around too long in the stomach causing an over production of acid.
 If you are enzyme deficient, you are not absorbing nutrients from your food, even if the food you are eating is very healthy.
If you are enzyme deficient, you are not absorbing nutrients from your food, even if the food you are eating is very healthy. - In addition to not being able to absorb nutrients from what you are eating, enzyme deficiency can also cause many digestive symptoms such as acid reflux, heartburn, indigestion, nausea and vomiting, constipation, and diarrhea.
- At birth we are given a certain potential for manufacturing enzymes in our body, creating an enzyme “reserve.” However, if we do not continually replenish that reserve through proper nutrition, it runs out. With every decade of life our enzyme production depletes by 13%.
- Our digestive enzymes are called Everyday Enzymes™. They are what I like to call medical grade enzymes (high potency and no fillers). This is important when taking a supplement, especially digestive enzymes. It is meant to be taken with meals to help you digest your food better. Remember, digesting your food properly is the first step to not only eliminating digestive issues (especially Acid Reflux) but getting you off of over-the-counter and prescription meds (like PPI medicines) while at the same time giving you your life back.
- Greens Anyone struggling with Acid Reflux / GERD is probably also struggling with being tired and low energy. This is due to vitamin and mineral deficiencies. One of the easiest things you can do to counter that is take a pure vitamin and mineral supplement.
 Our Greens supplement is called Gastro Greens™. These are also medical grade (high potency and no fillers). It contains green food that has been dried and pulverized and put into a capsule. We dose 3 per day; it doesn’t matter when you take them, all 3 at the same time or 1 with every meal.
Our Greens supplement is called Gastro Greens™. These are also medical grade (high potency and no fillers). It contains green food that has been dried and pulverized and put into a capsule. We dose 3 per day; it doesn’t matter when you take them, all 3 at the same time or 1 with every meal. - These are meant to take the place of a standard one-a-day multi-vitamin because your body wants to get vitamins and minerals from real food not synthetic capsules made in a lab.
- I also encourage you to get off gummy vitamins. They may taste good, but they are loaded with sugar / artificial sugar and are doing more damage to the body than good
- Green food is what builds the body, it’s what builds the blood. If you’re not eating a lot of green this is a great way to supplement it. And if you are eating green, this is a great way to get even more into the body every day. The vegetables we eat today are less nutritious than the vegetables our grandparents ate due to our soil being depleted. Anything you can do to get more vitamins and minerals in the body, the better.
- Increase your daily dose of Gastro Greens™ each day if you are sick or hurt, it will speed up your recovery time.
-
 Alkaline Water The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
Alkaline Water The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
- Just like a fish tank or a swimming pool, our body needs to maintain a certain pH to stay healthy. If we get really sick and are in the hospital, our pH is monitored because if it drops below a certain amount we can die. When we are healthy, we don’t pay much attention to our pH, but that doesn’t mean it’s not important. On the pH scale, our body is slightly alkaline, so anything you can do to drink and eat more alkaline makes it easier for your body to maintain its alkalinity and in turn work to keep you healthy.
- Your body is a healing vessel, it wants you to be well. Sometimes we just need to help it out a little. Drinking alkaline water is one simple thing you can do to help your body out. It’s especially helpful for people suffering from Acid Reflux / GERD because it helps to maintain the acid alkaline balance in the stomach.
 Chop, Chop! Cookbook many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
Chop, Chop! Cookbook many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
- The book is available in English and Spanish.
As a disclaimer, it’s important to say that if a patient’s GERD has progressed to Barrett’s Esophagus it is important to remain on a PPI for life. You must make sure at all costs acid does not continue to reflux into the esophagus damaging the tissue further. To slow down the long-term side effects of the PPI, I encourage those patients more than ever to follow the holistic regimen I’ve laid out above. If you’re going to be on a PPI for life, you need all the help you can get with digesting your food and nutrient absorption.
Act Now – 3 Options to Move in the Right Direction
Depending on your level of commitment and interest in turning around your Acid Reflux issues, there are three options to consider:
- Good if you want to start slow and are not sure if this is for you, at least order our Everyday Enzymes™ , Gastro Greens™ , and Chop, Chop! Cookbook. The investment is minimal and it’s not hard to incorporate these two supplements into your daily routine to see if they can help. I do encourage you to try this regimen for at least 3 months before you decide it’s not working for you. Doing something for only a few days or even a month is not going to make a huge difference in your body, especially if you’ve been struggling with Acid Reflux for a long time.
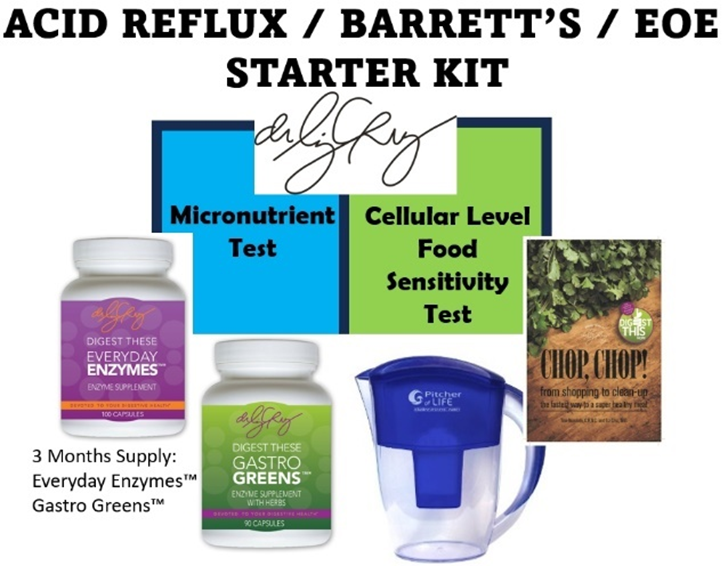
- Better if you are ready to make a more serious commitment to turning around your Acid Reflux and have some money to invest in yourself, consider ordering our Acid Reflux Starter Kit . It includes three months’ worth of our Everyday Enzymes™, Gastro Greens™, and the Chop, Chop! Cookbook, along with an Alkaline Water Pitcher so you can start benefiting from alkaline water right away. In addition, it also comes with the Cellular Level Food Sensitivity Test and the Micronutrient Test I explained above. By purchasing the kit, you get all these items at a discounted rate so it’s much better than buying them individually.
- Best if you have money to invest in yourself, are suffering from other medical issues aside from just Acid Reflux and you’re sick and tired of feeling sick and tired consider going all in on our Digestive Revolution™ Ultimate Plan. This is my 4-Step Proprietary System which is an outcomes and scientific based system that starts at the cellular level. The system delivers 4 main outcomes:
- Eliminates digestive issues such as gas, bloating, constipation, diarrhea, and acid reflux.
- Removes pain and inflammation from the body.
- Reduces the need for prescription and over-the-counter medications.
- Increases energy, enhances sleep, and the ability to get to your healthy base weight.

No matter what you decide to do, do something! You get sick and remain sick by accident – you get healthy on purpose!
References
[1] NIH - https://www.niddk.nih.gov/health-information/digestive-diseases/constipation/definition-facts
[2] Johns Hopkins medicine website - https://www.hopkinsmedicine.org/health/conditions-and-diseases/constipation
[3] BMC Public Health - https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-14-374
[4] National Library of Medicine - https://pubmed.ncbi.nlm.nih.gov/12739323/
[5] John’s Hopkins Medicine - https://www.hopkinsmedicine.org/health/conditions-and-diseases/constipation
[6] Medical News Today - https://www.medicalnewstoday.com/articles/bristol-stool-scale
[7] Cleveland Clinic - https://my.clevelandclinic.org/health/diseases/13177-anal-fissures
These statements have not been evaluated by the Food and Drug Administration.
These products are not intended to diagnose, treat, cure, or prevent any disease.

Liz Cruz, MD
- Award-winning, board-certified gastroenterologist
- Sought-after leader in solving complex digestive health conditions
- 30+ years of dedicated patient service
- Best-selling author, podcaster and international speaker
Dr. Liz Cruz was named Top Gastroenterologist in 2019. She is a Diplomat of the American Board of Internal Medicine and the American Board of Gastroenterology. Dr. Cruz is a member of the American Gastroenterological Association, American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. In 2014, she received the Quilly Award from the National Academy of Best-Selling Authors® for her Best-Selling Book “Answering the Call".
