Interesting Statistics Regarding Fatty Liver
-
 Experts estimate about 24% of U.S. adults have NAFLD (nonalcoholic fatty liver disease).
Experts estimate about 24% of U.S. adults have NAFLD (nonalcoholic fatty liver disease).
- About 1.5% to 6.5% of U.S. adults have NASH (nonalcoholic steatohepatitis).1
- In the United States, over 64 million people are projected to have NAFLD, with annual direct medical costs of about $103 billion ($1,613 per patient).2
- Left untreated, Fatty Liver can progress into liver cirrhosis and in 2023, 56,585 died from liver cirrhosis up from 47,919 in 2019.3
Definition of Fatty Liver
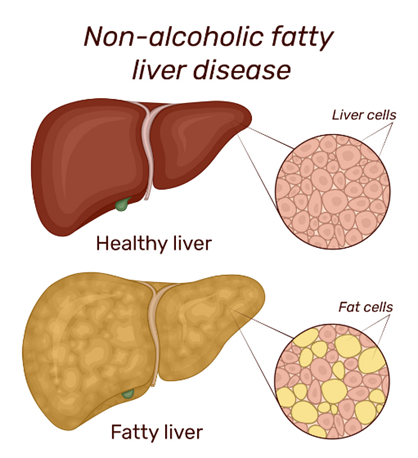
Your liver is the largest organ inside your body. It helps your body digest food, store energy, and remove toxins/poisons. Fatty liver disease is a condition in which fat builds up in your liver. There are two main types:
- Nonalcoholic fatty liver disease (NAFLD)
- Alcoholic fatty liver disease, also called alcoholic steatohepatitis
Nonalcoholic fatty liver disease (NAFLD) is a condition in which excess fat builds up in your liver. This buildup of fat is not caused by heavy alcohol use. When heavy alcohol use causes fat to build up in the liver, this condition is called alcohol-associated liver disease (ALD).
Two types of NAFLD are nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). People typically develop one type of NAFLD or the other, although sometimes people with one form are later diagnosed with the other form of NAFLD.
NAFL
NAFL is a form of NAFLD in which you have fat in your liver but little or no inflammation or liver damage. NAFL typically does not progress to cause liver damage or complications. However, NAFL can cause pain from enlargement of the liver.
NASH
NASH is the form of NAFLD in which you have inflammation of the liver and liver damage, in addition to fat in your liver. The inflammation and liver damage of NASH can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis, in which the liver is scarred and permanently damaged. Cirrhosis can lead to liver cancer.
Experts are not sure why some people with NAFLD have NASH while others have NAFL. NAFLD is one of the most common causes of liver disease in the United States. Most people with NAFLD have NAFL. Only a small number of people with NAFLD have NASH.
About 10% of children in the U.S. have NAFLD – and numbers are growing as the number of obese kids grows. But most children with NAFLD don't get liver problems – and NAFLD can be controlled or reversed if your child changes their lifestyle and eating habits.
Causes of Fatty Liver
Experts don't know exactly why fat builds up in some livers and not others. They also don't fully understand why some fatty livers turn into NASH.4
NAFLD and NASH are both linked to the following:
- Genetics
- Overweight or obesity.
- Insulin resistance, which happens when your cells don't take up sugar in response to the hormone insulin.
- Type 2 diabetes, sometimes called high blood sugar or hyperglycemia.
- High levels of fats, especially triglycerides, in the blood.
These combined health problems may contribute to a fatty liver. However, some people get NAFLD even if they do not have any risk factors. Many diseases and health problems can increase your risk of NAFLD, including:
-
 Family history of fatty liver disease or obesity.
Family history of fatty liver disease or obesity. - Growth hormone deficiency, which means the body doesn't make enough hormones to grow.
- High cholesterol.
- High levels of triglycerides in the blood.
- Insulin resistance.
- Metabolic syndrome.
- Obesity, especially when fat is centered in the waist - research suggests that NAFLD is present in up to 75% of people who are overweight and in more than 90% of people who have severe obesity.5,6
- Polycystic ovary syndrome.
- Obstructive sleep apnea.
- Type 2 diabetes - studies suggest that one-third to two-thirds of people with type 2 diabetes have NAFLD.
- Underactive thyroid, also called hypothyroidism.
- Underactive pituitary gland, or hypopituitarism.
NASH is more likely in these groups:
- People older than 50.
- People with certain genetic risk factors.
- People with obesity.
- People with diabetes or high blood sugar.
- People with symptoms of metabolic syndrome, such as high blood pressure, high triglycerides and a large waist size.
While NAFLD occurs in people of all races and ethnicities, it is most common among Hispanic individuals, followed by non-Hispanic whites and Asian Americans, including those of East Asian and South Asian descent.7,8
It is hard to tell NAFLD from NASH apart without a clinical evaluation and testing.
Symptoms of Fatty Liver
NAFLD often has no symptoms. When it does, they may include:
- Fatigue
- Not feeling well, or malaise
- Pain or discomfort in the upper right belly area.
Possible symptoms of NASH and cirrhosis, or severe scarring, include:
If you have any questions at all about whether the pain you’re experiencing is gas or a serious condition, see a healthcare provider.
Although gas pain is usually harmless, it can signal a genuine problem with your digestive system. If you are experiencing excess gas or gas pain along with any of the following symptoms, don’t dismiss it. See a healthcare provider.
Symptoms to be on the lookout for, alongside gas pain, include:
- Itchy skin.
- Abdominal swelling, also called ascites (uh-SY-teez).
- Shortness of breath.
- Swelling of the legs.
- Larger-than-normal breasts in men.
- Spider-like blood vessels just beneath the skin's surface.
- Enlarged spleen.
- Red palms.
- Yellowing of the skin and eyes, or jaundice.
- Nausea, weight loss, or loss of appetite
- Tiredness or mental confusion
How Fatty Liver is Diagnosed
Because most people don’t have symptoms, these conditions aren’t easy to diagnose.9
Your doctor may use different methods to find out if you have fatty liver disease. Some of the things your doctor may use to diagnose fatty liver disease are:
Health History and Physical Exam
Your doctor will ask about your alcohol use. This information can help your doctor tell if you have ALD (alcohol-associated liver disease) or NAFLD, so be truthful. They’ll also ask about medications you take, how you eat, and other health conditions you might have. Your doctor will also:
- Check your body for signs of liver problems such as an enlarged liver or jaundice.
- Check your height and weight to calculate your body mass index (BMI). Your BMI determines how much you should weigh based on your height.
Blood Tests
Your doctor may order the following blood tests:
 Liver function and liver tests to detect and monitor liver disease and damage. The cells in your liver have proteins called enzymes. When these cells are damaged, the enzymes leak into your bloodstream, where they can be measured. If your liver is damaged, the level of these enzymes will be higher than normal.
Liver function and liver tests to detect and monitor liver disease and damage. The cells in your liver have proteins called enzymes. When these cells are damaged, the enzymes leak into your bloodstream, where they can be measured. If your liver is damaged, the level of these enzymes will be higher than normal.- Fibrosis assessment tests to estimate your level of liver scarring (fibrosis). There are blood tests that can provide a score to determine the amount and stage of fibrosis in the liver.
- Lipid profile to measure blood fats, such as cholesterol and triglycerides.
- Other blood tests to rule out other causes of fatty liver, like tests for hepatitis C and Wilson disease (a rare genetic condition).
- Hemoglobin A1c, which shows the stability of your blood sugar.
Imaging Tests
You may get an ultrasound, computerized tomography (CT) scans, or magnetic resonance imaging (MRI). These tests can show if there’s any fat in your liver. But they can’t tell whether you have simple fatty liver or NASH. There are some tests that can show whether you have fibrosis by measuring the stiffness of your liver. When liver cells die, they are replaced by scar tissue, which is stiff. The stiffer your liver is, the more scarring there will be.
- Transient elastography measures liver stiffness using a special ultrasound machine.
- Magnetic resonance elastography (MRE) combines ultrasound and MRI to create a visual map of stiffness throughout your liver.
Liver Biopsy
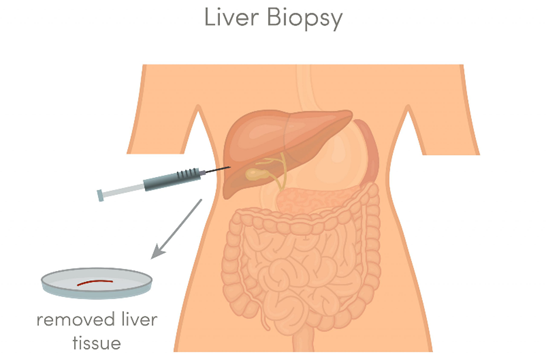 Not everyone with NAFLD needs to have a liver biopsy. Your doctor may recommend it if you are at risk for NASH or if other tests show that you may have NASH complications such as cirrhosis. A doctor removes a sample of tissue from your liver and sends it to a lab to see if you have liver inflammation or damage. You’ll get this done at a hospital or outpatient surgery center. Before the procedure, you’ll get medicine to help you relax or control pain. For the biopsy, your doctor numbs the area and uses a special needle to take a small piece of tissue from your liver. A liver biopsy is the only way for doctors to diagnose NASH.
Not everyone with NAFLD needs to have a liver biopsy. Your doctor may recommend it if you are at risk for NASH or if other tests show that you may have NASH complications such as cirrhosis. A doctor removes a sample of tissue from your liver and sends it to a lab to see if you have liver inflammation or damage. You’ll get this done at a hospital or outpatient surgery center. Before the procedure, you’ll get medicine to help you relax or control pain. For the biopsy, your doctor numbs the area and uses a special needle to take a small piece of tissue from your liver. A liver biopsy is the only way for doctors to diagnose NASH.
Types of Fatty Liver
There are two main types of fatty liver disease:
1. Nonalcoholic Fatty Liver Disease (NAFLD)
This type is very common in the U.S., affecting 1 in 3 adults. Unlike the other main type, you don't get it from drinking alcohol. There are two forms of NAFLD:
- Simple fatty liver: This means you have fat in your liver, but you may not have any inflammation in your liver or damage to your liver cells. It usually doesn’t get worse or cause problems with your liver. Most people with NAFLD have simple fatty liver.
- Nonalcoholic steatohepatitis (NASH):This is much more serious than simple fatty liver. NASH means you have inflammation in your liver. The inflammation and liver cell damage that happen with NASH can cause serious problems such as fibrosis and cirrhosis, which are types of liver scarring, and liver cancer. These problems can lead to liver failure and require a liver transplant. About 20% of people with NAFLD have NASH.
2. Alcohol-Related Fatty Liver Disease (ALD)
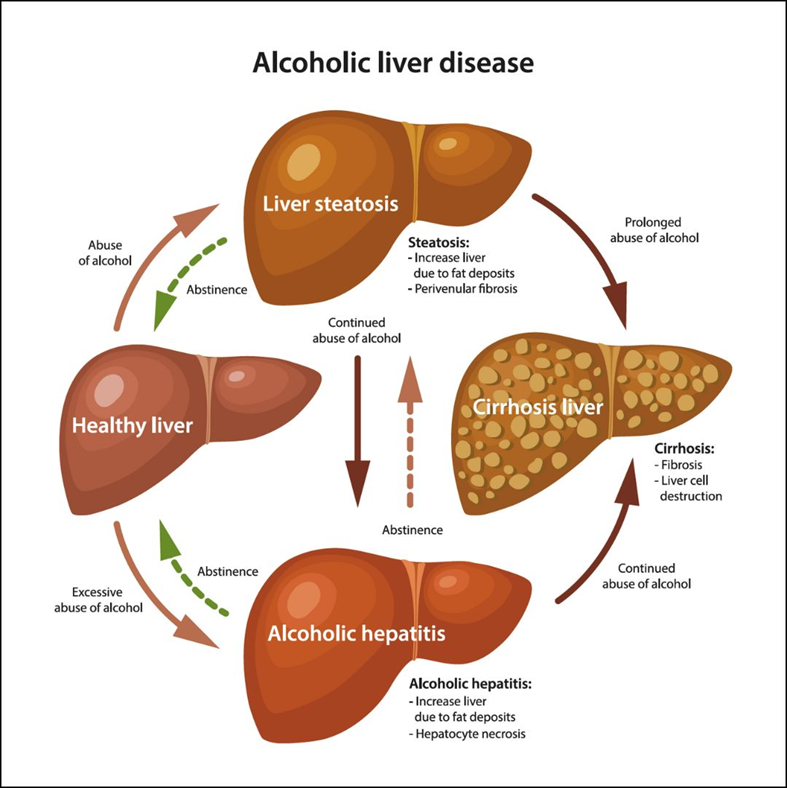 This type is less common, affecting about 5% of people living in the U.S., and is caused by drinking alcohol. For this reason, it usually gets better when you stop drinking alcohol. If you keep drinking, ALD can cause serious problems. These include:
This type is less common, affecting about 5% of people living in the U.S., and is caused by drinking alcohol. For this reason, it usually gets better when you stop drinking alcohol. If you keep drinking, ALD can cause serious problems. These include:
- Enlarged liver. It doesn’t always cause symptoms, but you may have pain or discomfort on the upper right side of your belly.
- Alcoholic hepatitis. This is swelling in the liver that can cause fever, nausea, vomiting, belly pain, and jaundice (yellowish skin and eyes).
- Alcoholic cirrhosis. This is a buildup of scar tissue in your liver. It can cause the same symptoms as alcoholic hepatitis, plus:
- Large amounts of fluid buildup in your belly (ascites)
- High blood pressure in the liver
- Bleeding in your body
- Confusion and changes in behavior
- Enlarged spleen (a small organ inside your rib cage that's part of your immune system)
- Liver failure, which can be fatal
Alcohol-related fatty liver disease usually comes first. It can then get worse and become alcoholic hepatitis. Over time, it may turn into alcoholic cirrhosis. If you drink heavily, talk with your doctor. It’s confidential, and they can help you get your drinking under control to save your health.
Traditional Medical Treatment for Fatty Liver
The one good thing about Fatty Liver disease is that it can be reversed. The liver is one of the few organs in your body that can replace damaged tissue with new cells rather than with scar tissue. But that reversal only works if you stop damaging the liver.
There are no medications approved for Fatty Liver. Usually, the first line of treatment is to lose weight. It helps reduce fat, inflammation, and scarring in your liver. Losing just 3% to 5% of your body weight can cut down on how much fat is in your liver.
You’ll also need to quit drinking. It’s the only way you can keep liver damage from getting worse. You may even be able to undo some of the liver damage that’s already happened. Talk to your doctor about how you can get help. You may need a medically supervised detox program to safely quit drinking and manage withdrawal symptoms.
If you have complications due to NASH, such as cirrhosis or liver failure, you may need to have a liver transplant. In general, people with NASH who get a liver transplant do very well.
Lifestyle changes can help:
- Exercise more. Try to be active at least 30 minutes a day most days of the week. If you're trying to lose weight, you might find that it helps to exercise more than this. But if you don't already exercise regularly, get your doctor's OK first and start slowly.
- Be kind to your liver. Don’t do things that will make it work harder. Skip alcohol. Take medications and over-the-counter drugs only as instructed.
- Get your cholesterol down. Eat a healthy plant-based diet, exercise, and take your medications. This will get – and keep – your cholesterol and your triglyceride levels where they need to be.
- Manage your diabetes. Check your blood sugar and take medications as your doctor prescribes.
- Change your diet.Changing the way you eat can help to lessen or reverse NAFLD or NASH.
 Limit foods that are high in fats (such as sausage, bacon, cake, chocolate, etc.).
Limit foods that are high in fats (such as sausage, bacon, cake, chocolate, etc.).- Replace saturated fats (such as butter, red meat, and cheese) with unsaturated fats (such as olive oil, salmon, and avocado).
- Eat foods with a low glycemic index, such as fruits, vegetables, and whole grains.
- Avoid foods and drinks with a lot of simple sugars (such as sweetened sodas, sports drinks, juices, and ice cream).
- Follow a Mediterranean diet.
Complications of Fatty Liver
Severe liver scarring, or cirrhosis, is the main complication of NAFLD and NASH. Cirrhosis happens because of liver injury, such as the damage caused by chronic inflammation in NASH. As the liver tries to stop inflammation, it creates areas of scarring, also called fibrosis. With ongoing inflammation, fibrosis spreads and takes up more liver tissue.
If nothing is done to stop the scarring, you can develop cirrhosis which then can lead to:
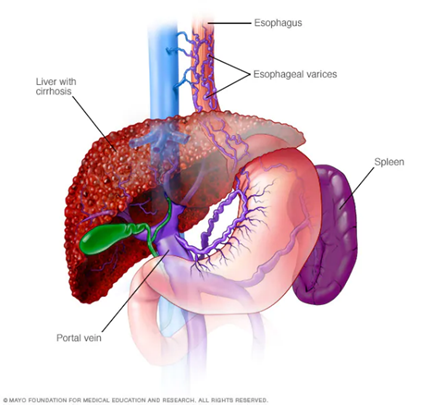 Fluid buildup in the stomach area, called ascites.
Fluid buildup in the stomach area, called ascites.- Swollen veins in your esophagus, or esophageal varices which can rupture and bleed.
- Confusion, sleepiness, and slurred speech, also called hepatic encephalopathy.
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- Liver cancer.
- End-stage liver failure, which means the liver has stopped working.
If cirrhosis leads to liver failure, you may need a liver transplant. People with NASH have an increased chance of dying from liver-related complications.
People with NAFLD have a higher risk for certain health problems, including:
- cardiovascular disease, which is the most common cause of death in people who have NAFLD
- type 2 diabetes
- metabolic syndrome
- Overactive spleen, or hypersplenism, which can cause too few blood platelets.
- conditions that may be part of metabolic syndrome, such as high blood pressure and abnormal levels of fats—cholesterol and triglycerides—in the blood.
What Traditional Medicine is Not Telling You About Fatty Liver
The information I am about to share with you was not taught to me during any of my medical training. What medical school, internship, internal medicine residency, and my Gastroenterology fellowship taught me was how to diagnose symptoms, prescribe medicines and do amazing colonoscopies and upper endoscopies. What it didn’t teach was the true reason why people are having symptoms to begin with. There is a reason why there are no medications for Fatty Liver – that is because medications do more harm to the liver than good.
Even in traditional medicine the main way to repair or reverse a Fatty Liver is to make lifestyle changes. This is wonderful to hear, but there are some things I’ve learned over the last several years regarding detoxing the body and incorporating certain vitamins and herbs to help support and repair the liver that traditional medicine doesn’t address just yet.
Having a healthy functioning liver offers many benefits to the body including, but not limited to, proper digestive system functionality, improved skin health and texture, increased mental clarity, and a noticeable boost in overall energy levels.
As I mentioned earlier, your liver is your largest detoxing organ. The liver regulates most chemical levels in the blood and excretes a product called bile. This helps carry away waste products from the liver. All the blood leaving the stomach and intestines passes through the liver. The liver processes this blood and breaks down, balances, and creates the nutrients. In addition, it metabolizes drugs into forms that are easier to use for the rest of the body. More than 500 vital functions have been identified with the liver.
When the liver has broken down harmful substances, its by-products are excreted into the bile or blood. Bile by-products enter the intestine and leave the body in the form of feces. Blood by-products are filtered out by the kidneys and leave the body in the form of urine. Everything you consume – food, drinks, medicines, skin products, goes through the liver at some point.
 Now consider the Standard American Diet (SAD), loaded with processed foods, fast foods, fancy coffees, and energy drinks. All these items are filled with chemicals, preservatives, dyes, sugars, and even worse, artificial sugars, items our body doesn’t even know what to do with much less process properly. Imagine the damage being done to the liver as it works hard to process these items.
Now consider the Standard American Diet (SAD), loaded with processed foods, fast foods, fancy coffees, and energy drinks. All these items are filled with chemicals, preservatives, dyes, sugars, and even worse, artificial sugars, items our body doesn’t even know what to do with much less process properly. Imagine the damage being done to the liver as it works hard to process these items.
Now consider all the over the counter and prescription medications people are taking. The number of U.S. adults who report taking at least one prescription medication per day is now 70%, a 14 percentage-point increase from 2019 data.10 And this doesn’t even take into account over the counter pain medicines, ie. NSAIDS (ie Ibuprofen, Advil, Motrin, etc.) which I know many of my patients take on a regular basis. No matter what medicine you are taking, including pain medicine, it is a toxic chemical you are putting in your body that your liver must process. Is it any wonder why almost 30% of adults are being diagnosed with Fatty Liver?
So aside from cleaning up your diet, consuming less alcohol, nicotine and drugs, and getting to the bottom of your symptoms to help eliminate the need for medicines, what else can be done? The answer is regularly detoxing the body and taking vitamins and herbs to help support the liver and its function.
Why it’s Important to Detoxify Your Body
If you had asked me 15 years ago about the importance of detoxing the body, I would have referred you to a naturopathic doctor, but today it is my favorite topic to discuss. As a Gastroenterologist one of my favorite organs (the colon) is responsible for much of that detoxification. Our body has many natural mechanisms for detoxing, for example urine, stool, sweat, and breath. As we age, our body slows down, and we aren’t detoxing like we should. Every day we are being exposed to toxins in the air we breathe, stuff we put on our skin, the food we eat, the drinks we drink and the medicine we take. Over time, as our body slows down, we hold on to more of these toxins making us tired and sluggish.
I have patients in their early 20’s that are experiencing the tired and low energy issue because this is a generation of kids of that have lived off processed foods, fast foods, energy drinks, fancy coffees, recreational drugs, vapes, etc. Imagine the toxins their bodies take in every day and even though they are young, their body can’t keep up.
Our body is a healing vessel, it wants us to be well, but when we continue to expose it to toxins day in and day out, it can only do so much. At some point it’s going to throw up its hands and say “enough is enough, you’re on your own!” This is when symptoms like aches, pains, tiredness, low energy, foggy brain, set in. And unfortunately, when this happens the pharmaceutical and food industry will tell us to take pain meds or drink more caffeine. In the end, adding more toxicity to the body - it truly is an endless cycle.
Every bit of toxins we breathe in, or put in or on our body, runs through our liver, as I stated earlier causing almost 30% of adults being diagnosed with Fatty Liver – and these are the people that go to their doctor’s office. Who knows how many people that are out there don’t even go to the doctor. I have several friends that haven’t been to their doctor in decades because they say they “feel fine” yet are taking pain meds every day for one reason or another.
The bottom line is, we are all moving in the same direction, it just depends on how fast you want to get there. Keeping a clean body is one way to slow the process of aging and help get you off unnecessary prescription and over the counter medicines. Yet one more step to reversing a Fatty Liver.
Vitamins and Herbs for a Healthy Liver
Many studies have been done over the years on liver disease, specifically one’s that try to link vitamin and / or mineral deficiencies to the progression of the disease leading to death. Just a few examples are as follows:
- A deficiency in Vitamin A, a fat-soluble vitamin that includes retinol and carotenoids, has been associated with various liver diseases and the higher overall mortality.11
- Choline is a vital nutrient that helps your liver and brain function correctly. A choline supplement may help reduce your risk of fatty liver disease.12
- N-acetyl cysteine (NAC) plays a role in the detoxification of your kidneys and liver. It can help to prevent potential side effects of drugs and environmental factors — such as exposure to heavy metals — that may impact these organs.13
- Studies show that selenium levels in fatty liver patients are lower than normal. Selenium can effectively alleviate metabolic disorders by relieving anti-oxidative stress and anti-inflammatory regulation.15
There have also been many studies that show certain herbs have a positive effect on supporting the liver and reversing liver cell regeneration. A couple examples are as follows:
 Milk thistle, scientifically known as Silybum marianum, is an herb traditionally used to support liver health. The primary active compound in milk thistle is silymarin, a mixture of flavonolignans that exhibit antioxidant, anti-inflammatory, and antifibrotic properties. Silymarin is believed to support liver function by reducing oxidative stress, promoting liver cell regeneration, and providing a protective barrier against harmful substances that can damage the liver.
Milk thistle, scientifically known as Silybum marianum, is an herb traditionally used to support liver health. The primary active compound in milk thistle is silymarin, a mixture of flavonolignans that exhibit antioxidant, anti-inflammatory, and antifibrotic properties. Silymarin is believed to support liver function by reducing oxidative stress, promoting liver cell regeneration, and providing a protective barrier against harmful substances that can damage the liver.
- Clinical studies have backed the hepatoprotective effects of milk thistle. Research has shown that silymarin can aid in slowing the progression of liver diseases such as alcoholic hepatitis, cirrhosis, and non-alcoholic fatty liver disease. Furthermore, it can enhance the detoxification processes, reinforcing the liver's ability to process and remove toxins from the body.14
-
 Dandelion is a medicinal herb that has been used for centuries to treat a wide range of health conditions. It is rich in antioxidants and has properties that can help flush out toxins from the liver and reduce inflammation. It can heal the damage caused by liver ailments and most importantly can boost liver function / bile production and enhancing the body's natural detoxing processes.14
Dandelion is a medicinal herb that has been used for centuries to treat a wide range of health conditions. It is rich in antioxidants and has properties that can help flush out toxins from the liver and reduce inflammation. It can heal the damage caused by liver ailments and most importantly can boost liver function / bile production and enhancing the body's natural detoxing processes.14
A Different Approach to Fatty Liver
In 2007, I approached my wife and Office Manager Tina and told her how frustrated I was with medicine. I was running all the tests, doing all the procedures, and prescribing all the medicines and could not figure out why my patients were still hurting. That frustration led us on a two-year journey to learn what my medical degree did not teach me about the body and how it works, in addition to what is happening in the medical industry, pharmaceutical industry and food industry to cause so many health problems in our society.
After we learned what we did, we felt obligated to share this with our patients and we’ve been doing so since 2010. Tina was so passionate about what we learned, she went back to school and received her Certificate in Holistic Nutrition so she could help me deliver this message to as many people as we possibly could. Since we started on this journey, we have helped tens of thousands of patients and wellness clients eliminate their symptoms naturally, helping their bodies work again like they were meant to work.And the best part of it all, is it’s not as hard as you may think to turn it all around, no matter how long you’ve been suffering or how old you are. If you are willing to put in the time, effort and invest in yourself, you can have your life back too.
Fatty Liver is so prevalent today but the great thing about it is it can be reversed. Although lifestyle changes are important for this to occur there are some other ways to help speed the process up. Below is the plan I use with my patients that helps get to the bottom of their issues so we can detoxify and rebuild the liver as fast as possible.
Details on this approach are as follows:
 A Cellular Level Food Sensitivity Test Anyone diagnosed with Fatty Liver absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
A Cellular Level Food Sensitivity Test Anyone diagnosed with Fatty Liver absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
- Traditional allergists run skin and blood tests to determine food allergies. This food sensitivity test goes a level deeper to study the cellular level of the body, the difference between a food allergy and a food sensitivity.
 Micronutrient Test This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
Micronutrient Test This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
- This test is the ultimate guide to what foods and supplements you should and shouldn’t be consuming to offset your deficiencies. This test will give you the answer to why you are tired and have low energy. It is your chance to find out if all those supplements you are taking are necessary. Once you know what your cells really need, it becomes clear on how to replenish them.
- Protease Enzymes Proteolytic enzymes, also called protease, break down proteins in the body. If you are familiar with digestive enzymes you know that protease is just one of many enzymes that help break down the food we eat on a daily basis. However, protease enzymes go even further by helping to break down proteins throughout the whole body. The formulation of protease enzymes found in our Delicate Detox™ is designed to work only in the blood (on the whole-body level) instead of just in the stomach. What good do protease enzymes do in the blood; you may ask? Well, just about everything that makes us sick is either a protein or is protected by a protein.
 Bacteria, viruses, yeasts, and fungi are all protected by proteins. In addition, cancer cells are protected by proteins. Food allergens are also proteins. Many food allergies come from us not digesting our food well enough.
Bacteria, viruses, yeasts, and fungi are all protected by proteins. In addition, cancer cells are protected by proteins. Food allergens are also proteins. Many food allergies come from us not digesting our food well enough.- If we don’t have the proper digestive enzymes to break down our food on a daily basis and our food enters our small bowel partially digested, large protein molecules can get absorbed into the blood stream. This causes your immune system to kick-in and antibodies are formed with proteins to “protect” the body. Circulating Immune Complexes (CIC’s) are then formed. Basically, this means that your body has now created an immune response “tagged” to something that it shouldn’t. When this happens over and over, the body “stores” these “tags” into its own tissue, because it is now overwhelmed with trying to eliminate them through urination and sweat. This is why the body attacks its own tissue at times, as seen in diseases like lupus and rheumatoid arthritis. Supplementing with a proteolytic enzyme can help break down CIC’s, so that they can be passed through urine or sweat easily.
- The blood not only carries oxygen and nutrients throughout the body, it’s also a way for cells and organs to dispose of their garbage and dead material. One way to cleanse the blood is taking a protease enzyme supplement, which is capable of breaking down things that would otherwise compromise the immune system.
- In addition, these proteolytic enzymes can improve circulation by eating excess fibrin. Fibrin is a strong protein responsible for the development of blood clots. Excess fibrin makes the blood thick, which is a dangerous situation.
- As a result of cleaning out the blood the following can occur; inflammation is reduced, blood flow is optimized, blood clots are prevented, allergies are minimized, arterial plaque is dissolved, headaches are minimized, and cardiovascular health is optimized. Which is why when people start taking the Delicate Detox™ they are able to start fixing more than just their digestive system.
- There are not many supplements on the market that compare to our Delicate Detox™. Not only are they unique, but they are also what I like to call medical grade (high potency and no fillers). This is important when taking a supplement, especially protease enzymes. It is meant to be taken on an empty stomach. I usually take 2 when I wake up and 2 before going to bed.
- Liver Support although it is important to eat a cleaner diet, slow down on alcohol, nicotine and drugs, it never hurts to add a supplement to your daily routine that is specifically made to help support and repair the liver. Many of our patients have had great success with slowing down or reversing their Fatty Liver with daily supplementation.
 Our Liver supplement is called Love Thy Liver™. This formula promotes optimum liver as well as lymphatic system function by encouraging the normal removal of toxic materials and supporting the liver’s normal regeneration sequence.
Our Liver supplement is called Love Thy Liver™. This formula promotes optimum liver as well as lymphatic system function by encouraging the normal removal of toxic materials and supporting the liver’s normal regeneration sequence.- It includes a synergistic formulation of herbs (milk thistle and dandelion) and nutrients (N-Acetyl Cysteine) known for their ability to protect the liver, promote hepatic cell regeneration, and support detoxi¬cation.
- This product is the perfect choice to help counter exposure to various forms of environmental toxicity (the air we breathe, alcohol, nicotine, drugs, chemicals in food, drinks, skin products etc.)
- It’s also very effective when used to provide nutritional support before, during, and after a heavy metal detox or other types of aggressive cleanses.
-
 Alkaline Water The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
Alkaline Water The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
- Just like a fish tank or a swimming pool, our body needs to maintain a certain pH to stay healthy. If we get really sick and are in the hospital, our pH is monitored because if it drops below a certain amount we can die. When we are healthy, we don’t pay much attention to our pH, but that doesn’t mean it’s not important. On the pH scale, our body is slightly alkaline, so anything you can do to drink and eat more alkaline makes it easier for your body to maintain its alkalinity and in turn work to keep you healthy.
- Your body is a healing vessel, it wants you to be well. Sometimes we just need to help it out a little. Drinking alkaline water is one simple thing you can do to help your body out. It’s especially helpful for people who need to detox the body because it allows more water to absorb into the cells.
-
 Chop, Chop! Cookbook eating a cleaner diet is a huge step toward reversing Fatty Liver. Many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
Chop, Chop! Cookbook eating a cleaner diet is a huge step toward reversing Fatty Liver. Many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
- The book is available in English and Spanish.
Act Now – 3 Options to Move in the Right Direction
Depending on your level of commitment and interest in turning around your Fatty Liver, there are three options to consider:
- Good if you want to start slow and are not sure if this is for you, at least order our Delicate Detox™, Love Thy Liver™, and Chop, Chop! Cookbook. The investment is minimal and it’s not hard to incorporate these two supplements into your daily routine to see if they can help. I do encourage you to try this regimen for at least 3 months before you decide it’s not working for you. Doing something for only a few days or even a month is not going to make a huge difference in your body, especially if you’ve been struggling with Fatty Liver for a long time.
- Better if you are ready to make a more serious commitment to turning around your Fatty Liver and have some money to invest in yourself, consider ordering our Fatty Liver Starter Kit. It includes three months’ worth of our Delicate Detox™, Love Thy Liver™, and the Chop, Chop! Cookbook, along with an Alkaline Water Pitcher so you can start benefiting from alkaline water right away. In addition, it also comes with the Cellular Level Food Sensitivity Test and the Micronutrient Test I explained above. By purchasing the kit, you get all these items at a discounted rate so it’s much better than buying them individually.

- Best if you have money to invest in yourself, are suffering from other medical issues aside from just Fatty Liver and you’re sick and tired of feeling sick and tired consider going all in on our Digestive Revolution™ Ultimate Plan. This is my 4-Step Proprietary System which is an outcomes and scientific based system that starts at the cellular level. The system delivers 4 main outcomes:
- Eliminates digestive issues such as gas, bloating, constipation, diarrhea, and acid reflux.
- Removes pain and inflammation from the body.
- Reduces the need for prescription and over-the-counter medications.
- Increases energy, enhances sleep, and the ability to get to your healthy base weight.

No matter what you decide to do, do something! You get sick and remain sick by accident – you get healthy on purpose!
References
[1] NIH - https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts#:~:text=Experts%20estimate%20about%2024%25%20of,of%20U.S.%20adults%20have%20NASH.
[2] NIH - https://pubmed.ncbi.nlm.nih.gov/27543837/#:~:text=In%20the%20United%20States%2C%20over,billion%20(%241%2C613%20per%20patient).
[3] CDC - https://www.cdc.gov/nchs/fastats/liver-disease.htm
[4] Mayo Clinic - https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
[5] Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology. 2020;158(7):1851–1864. doi:10.1053/j.gastro.2020.01.052
[6] Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. Journal of Hepatology. 2006;45(4):600–606. doi: 10.1016/j.jhep.2006.06.013.
[7] Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi:10.1002/hep.29367
[8] Golabi P, Paik J, Hwang JP, Wang S, Lee HM, Younossi ZM. Prevalence and outcomes of non-alcoholic fatty liver disease (NAFLD) among Asian American adults in the United States. Liver International. 2019;39(4):748–757. doi:10.1111/liv.14038
[9] WebMD - https://www.webmd.com/hepatitis/fatty-liver-disease
[10] Civic Science - https://civicscience.com/a-growing-number-of-americans-report-taking-prescription-medications-daily/#:~:text=Recent%20CivicScience%20poll%20results%20reveal,point%20increase%20from%202019%20data.
[11] Hepatology Communications - https://journals.lww.com/hepcomm/fulltext/2023/05010/low_vitamin_a_levels_are_associated_with.12.aspx
[12] Cleveland Clinic - https://my.clevelandclinic.org/health/drugs/22202-choline-supplement
[13] Centre Spring MD - https://centrespringmd.com/nac-the-incredible-amino-acid-for-your-lungs-liver-and-longevity/#:~:text=NAC%20is%20also%20important%20for,%2C%20and%20arsenic%20(3).
[14] Rupa Health - https://www.rupahealth.com/post/top-4-herbs-for-liver-health-and-how-to-use-them-an-evidence-based-approach
[15] NIH - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9137657/#:~:text=The%20previous%20study%20shows%20that,has%20not%20been%20fully%20clarified.
These statements have not been evaluated by the Food and Drug Administration.
These products are not intended to diagnose, treat, cure, or prevent any disease.

Liz Cruz, MD
- Award-winning, board-certified gastroenterologist
- Sought-after leader in solving complex digestive health conditions
- 30+ years of dedicated patient service
- Best-selling author, podcaster and international speaker
Dr. Liz Cruz was named Top Gastroenterologist in 2019. She is a Diplomat of the American Board of Internal Medicine and the American Board of Gastroenterology. Dr. Cruz is a member of the American Gastroenterological Association, American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. In 2014, she received the Quilly Award from the National Academy of Best-Selling Authors® for her Best-Selling Book “Answering the Call".
