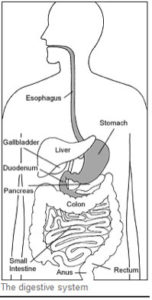
 Upper endoscopy enables the physician to look inside the esophagus, stomach, and duodenum (first part of the small intestine). The procedure might be used to discover the reason for swallowing difficulties, nausea, vomiting, reflux, bleeding, indigestion, abdominal pain, or chest pain. Upper endoscopy is also called EGD, which stands for esophagogastroduodenoscopy (eh-SAH-fuh-goh-GAS-troh-doo-AH-duh-NAH-skuh-pee).
Upper endoscopy enables the physician to look inside the esophagus, stomach, and duodenum (first part of the small intestine). The procedure might be used to discover the reason for swallowing difficulties, nausea, vomiting, reflux, bleeding, indigestion, abdominal pain, or chest pain. Upper endoscopy is also called EGD, which stands for esophagogastroduodenoscopy (eh-SAH-fuh-goh-GAS-troh-doo-AH-duh-NAH-skuh-pee).
For the procedure, a narrow, flexible, lighted tube called an endoscope (EN-doh-skope) will be inserted by your physician in through your mouth and advanced towards the back of your throat into the esophagus, stomach, and duodenum. Right before the procedure, the physician may spray your throat with a numbing agent that may help prevent gagging or more likely, you will receive pain medicine and a sedative to help you relax during the exam. The endoscope transmits an image of the inside of the esophagus, stomach, and duodenum, so the physician can carefully examine the lining of these organs. The physician places air in the stomach through the scope; this opens the folds of the stomach and makes it easier for the physician to examine the stomach lining.
With the endoscope, the physician can see abnormalities, like inflammation and bleeding, that don’t show up well on x-rays. The physician can also insert instruments into the scope to remove samples of tissue (biopsy) for further tests. In addition, heater probes or electrical probe can be inserted to help stop bleeding, and special medicines can be injected through the scope to help stop bleeding.
Possible complications of upper endoscopy include bleeding and puncture of the esophagus, stomach, and duodenal lining. These complications could require an emergent operation, however, such complications are rare. Most people will probably have nothing more than a mild sore throat after the procedure.
Although the examination will take approximately 30 minutes, plan on being with us about 1- 2 hours.
Preparation
Your stomach and duodenum must be empty for the procedure to be thorough and safe, so you will not be able to eat or drink anything for at least 6 hours beforehand. Also, you must arrange for someone to take you home–you will not be allowed to drive because of the sedatives. Please refer to your instructions that pertain to your scheduled examination. Preparation instructions differ based on the time of day your exam is scheduled.
On the day of your exam
Follow food and medication instructions that were given to you by our office. Have transportation arranged to take you home after your examination. Follow preparation instructions given to you for your scheduled exam.
It is important to bring with you the following items:
- Medication List
- Allergy List
- Medical problems and surgery list
- Insurance Information
- When you arrive please check in with the receptionist. A nurse will discuss you your medical history. Please let the nurse know if you are allergic to any medicines. The nurse will take your temperature, pulse, and blood pressure, and will place a small intravenous (IV) catheter in your arm vein for sedative medications to be given. You will be asked to sign a consent form authorizing the physician to perform the procedure.
Examination and before you go home
You will be observed closely by the nurses until you are awake. Many people do not recall any of the procedure because of the effect of the sedative medication. The doctor will speak with you before you leave. When the nursing staff assesses that you are ready to leave, you will be given final instructions. When you leave, you must leave with your transportation person.
After your examination at home
After you leave the outpatient center or hospital DO NOT DRIVE or operate mechanical equipment until the next day. Do not drink alcohol for 24 hours. You may eat and resume your normal activities, as you feel able unless otherwise instructed.





