Interesting Statistics Regarding Crohn’s and Colitis
- In 2019, the incidence of Crohn's disease was 10.7 new cases per 100,000 people, or about 33,000 new cases per year. The incidence of ulcerative colitis was 12.2 new cases per 100,000 people, or about 38,000 new cases per year.
- Approximately 1.6 million Americans currently have Irritable Bowel Disease (IBD), a growth of about 200,000 since the last time CCFA reported this figure (in 2011).1 IBD is the term used to represent both Crohn’s and Colitis.
- As many as 70,000 new cases of IBD are diagnosed in the United States each year.1
- There may be as many as 80,000 children in the United States with IBD. 1
Definition of Crohn’s and Colitis
Crohn’s disease and ulcerative colitis are inflammatory bowel diseases that cause chronic inflammation and damage in the gastrointestinal (GI) tract. The GI tract is responsible for digestion of food, absorption of nutrients, and elimination of waste. Inflammation impairs the ability of affected GI organs to function properly, leading to symptoms such as persistent diarrhea, abdominal pain, rectal bleeding, weight loss and fatigue.
While ongoing inflammation in the GI tract occurs in both Crohn’s disease and Ulcerative Colitis, there are important differences between the two diseases.
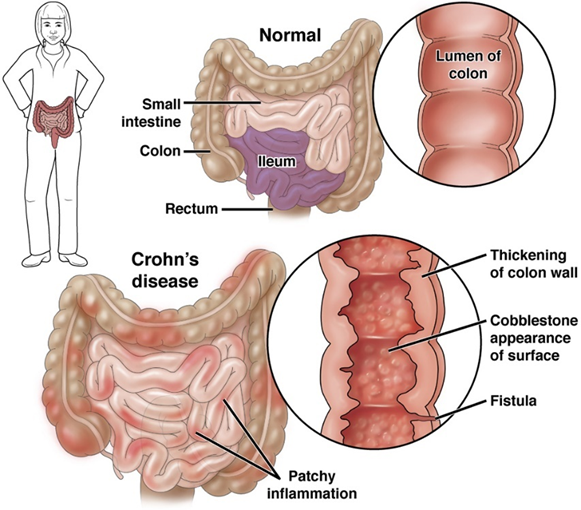
Crohn’s Disease
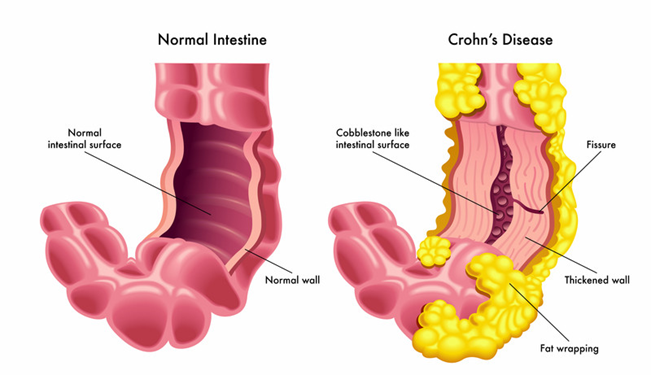
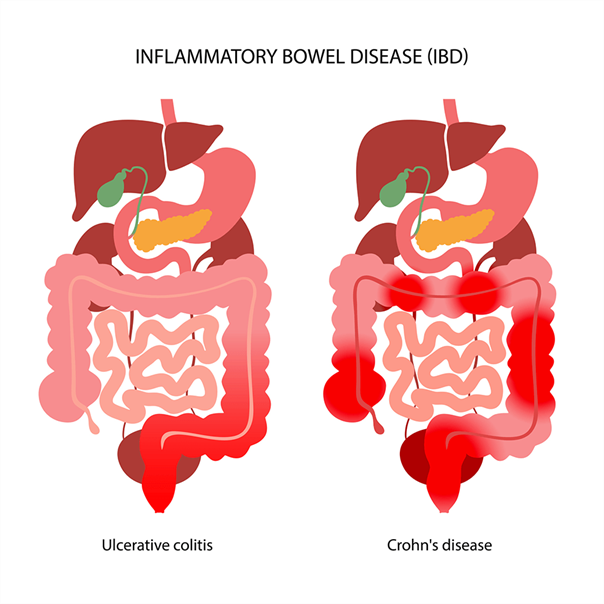 Crohn’s disease can affect any part of the GI tract, from the mouth to the anus. It most commonly affects the end of the small intestine (the ileum) where it joins the beginning of the colon. Crohn’s disease may appear in “patches,” affecting some areas of the GI tract while leaving other sections completely untouched. In Crohn’s disease, the inflammation may extend through the entire thickness of the bowel wall.
Crohn’s disease can affect any part of the GI tract, from the mouth to the anus. It most commonly affects the end of the small intestine (the ileum) where it joins the beginning of the colon. Crohn’s disease may appear in “patches,” affecting some areas of the GI tract while leaving other sections completely untouched. In Crohn’s disease, the inflammation may extend through the entire thickness of the bowel wall.
Ulcerative Colitis
Ulcerative Colitis is limited to the large intestine (colon) and the rectum. Inflammation occurs only in the innermost layer of the lining of the intestine. It usually begins in the rectum and lower colon but may also spread continuously to involve the entire colon.
Pseudomembranous Colitis - An inflammation of the colon associated with an overabundance of the bacterium Clostridioides difficile.
Ischemic Colitis -occurs when blood flow to the large intestine is temporarily reduced.
Radiation Colitis -results from exposure to radiation therapy.
Indeterminate Colitis -In some individuals, it is difficult to determine whether their IBD is Crohn’s disease or Ulcerative Colitis. In these rare cases, people are given the diagnosis of Indeterminate Colitis (IC).
Causes of Crohn’s and Colitis
While the exact cause of IBD is not entirely understood, it is known to involve an interaction between genes, the immune system, and environmental factors. The immune system usually attacks and kills foreign invaders, such as bacteria, viruses, fungi, and other microorganisms. However, in people with IBD, the immune system mounts an inappropriate response to the intestinal tract, resulting in inflammation.
This abnormal immune system reaction occurs in people who have inherited genes that make them susceptible to IBD. Unidentified environmental factors serve as the “trigger” that initiates the harmful immune response in the intestines.
 Experts think bacteria in your digestive tract can mistakenly trigger your immune system. This immune system response causes inflammation, leading to symptoms of IBD.2
Experts think bacteria in your digestive tract can mistakenly trigger your immune system. This immune system response causes inflammation, leading to symptoms of IBD.2
Aside from improper immune system response, researchers typically attribute the inflammation to poor diet, processed foods, and increased stress, which irritate inflammation and make IBD symptoms more severe. The following risk factors can cause individual cases of colitis: Bacterial or viral infections and food poisoning.3
Symptoms of Crohn’s and Colitis
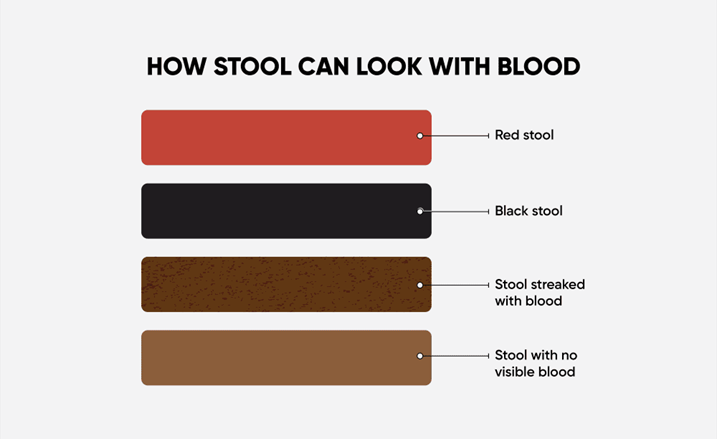
As the lining of the intestine becomes inflamed and ulcerated, it loses its ability to adequately process food and waste or absorb water, resulting in loose stools (diarrhea), and in severe cases weight loss. Most people with Crohn’s disease or Ulcerative Colitis experience an urgency to have a bowel movement and have crampy abdominal pain. Inflammation can cause small sores (ulcers) to form in the colon and rectum. These can join together and become large ulcers that bleed, resulting in bloody stools. Blood loss can eventually lead to anemia if unchecked.
The symptoms of IBD vary from person to person, may change over time, and can range from mild to severe. People with IBD often go through periods when the disease is quiet with few or no symptoms (remission), alternating with times when the disease is active and causing symptoms (flares).
Symptoms related to inflammation of the GI tract include:
- Diarrhea
- Bloody diarrhea
- Abdominal pain
- Rectal bleeding
- Urgent need to move bowels
- Sensation of incomplete evacuation
General symptoms that may also be associated with IBD:
- Fever
- Loss of appetite
- Weight loss
- Fatigue
- Nausea and Vomiting
- Night sweats
- Anemia
- Joint Pain / Soreness
- Skin changes that involve red, tender bumps under skin
- Eye Redness / Pain
- Loss of normal menstrual cycle
How Crohn’s and Colitis are Diagnosed
To help confirm a diagnosis of IBD, you will need a combination of tests and procedures:4
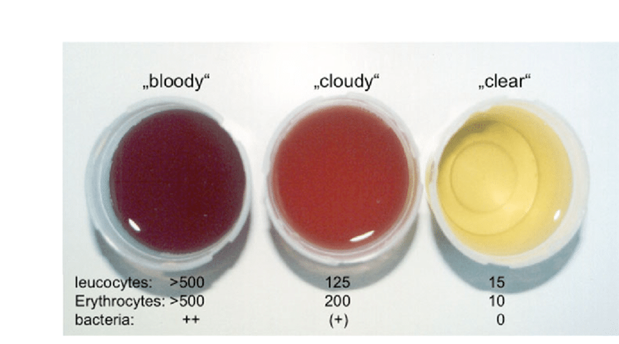
- Lab Tests: Your provider may suggest blood tests to check for anemia — a condition in which there aren't enough red blood cells to carry adequate oxygen to your tissues — or to check for signs of infection from bacteria or viruses.
- Stool Studies: You may need to provide a stool sample so that your provider can test for hidden (occult) blood or organisms, such as bacteria and parasites, in your stool.
- Endoscopic Procedures:
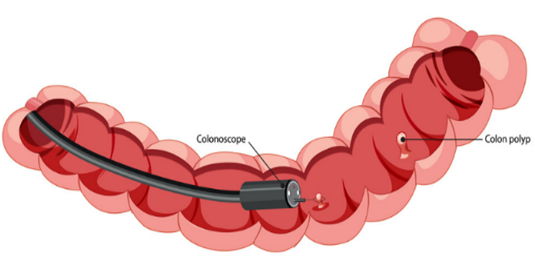 Colonoscopy. This exam allows your provider to view your entire colon using a thin, flexible, lighted tube with a camera at the end. During the procedure, small samples of tissue (biopsy) may be taken for laboratory analysis. A biopsy is the way to make the diagnosis of IBD versus other forms of inflammation.
Colonoscopy. This exam allows your provider to view your entire colon using a thin, flexible, lighted tube with a camera at the end. During the procedure, small samples of tissue (biopsy) may be taken for laboratory analysis. A biopsy is the way to make the diagnosis of IBD versus other forms of inflammation.- Flexible sigmoidoscopy. Your provider uses a slender, flexible, lighted tube to examine the rectum and sigmoid, the last portion of your colon. If your colon is severely inflamed, your provider may perform this test instead of a full colonoscopy.
- Upper endoscopy. In this procedure, your provider uses a slender, flexible, lighted tube to examine the esophagus, stomach and first part of the small intestine (duodenum). While it is rare for these areas to be involved with Crohn's disease, this test may be recommended if you are having nausea and vomiting, difficulty eating, or upper abdominal pain.
- Capsule endoscopy. This test is sometimes used to help diagnose Crohn's disease involving your small intestine. You swallow a capsule that has a camera in it. The images are transmitted to a recorder you wear on your belt, after which the capsule exits your body painlessly in your stool. You may still need an endoscopy with a biopsy to confirm a diagnosis of Crohn's disease. Capsule endoscopy should not be performed if a bowel obstruction is suspected.
 Balloon-assisted enteroscopy. For this test, a scope is used in conjunction with a device called an overtube. This enables the technician to look further into the small bowel where standard endoscopes don't reach. This technique is useful when a capsule endoscopy shows abnormalities, but the diagnosis is still in question.
Balloon-assisted enteroscopy. For this test, a scope is used in conjunction with a device called an overtube. This enables the technician to look further into the small bowel where standard endoscopes don't reach. This technique is useful when a capsule endoscopy shows abnormalities, but the diagnosis is still in question.- Imaging Procedures:
- X-ray. If you have severe symptoms, your provider may use a standard X-ray of your abdominal area to rule out serious complications, such as megacolon or a perforated colon.
- Computerized tomography (CT) scan. You may have a CT scan — a special X-ray technique that provides more detail than a standard X-ray does. This test looks at the entire bowel as well as at tissues outside the bowel. CT enterography is a special CT scan that provides better images of the small bowel. This test has replaced barium X-rays in most medical centers.
- Magnetic resonance imaging (MRI). An MRI scanner uses a magnetic field and radio waves to create detailed images of organs and tissues. An MRI is particularly useful for evaluating a fistula around the anal area (pelvic MRI) or the small intestine (MR enterography). Unlike CT, there is no radiation exposure with MRI.
Types of Crohn’s and Colitis
There are six main types of Crohn's disease, each with its own set of symptoms. Doctors define each type by the location of inflammation in your gastrointestinal tract (GI tract):5
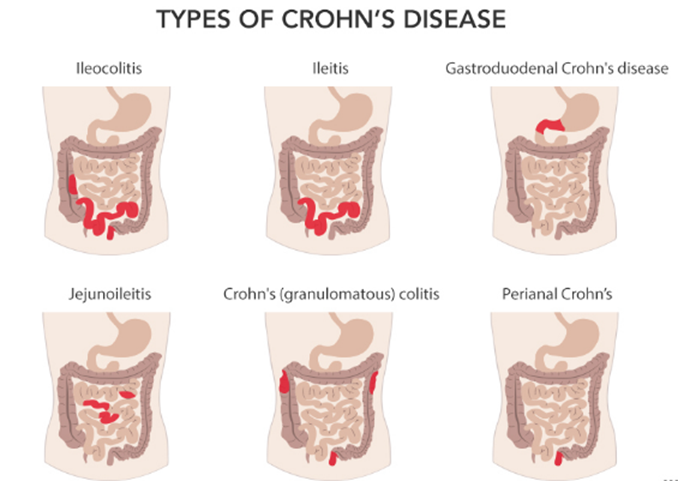
Ileocolitis:Inflames the end of the small intestine (ileum) and a portion of the large intestine (colon). This is the most common type of Crohn's disease. Symptoms you might have:
- Considerable weight loss
- Diarrhea
- Cramping
- Pain in the middle or lower right part of your abdomen
Ileitis:Inflames the last section of the small intestine (ileum). Symptoms you might have:
- Considerable weight loss
- Diarrhea
- Cramping
- Pain in the middle or lower right part of your abdomen
- Fistulas, or inflammatory abscesses, may form in the lower right section of your abdomen.
 Gastroduodenal Crohn’s: Inflames the stomach and the start of the small intestine (duodenum). Symptoms you might have:
Gastroduodenal Crohn’s: Inflames the stomach and the start of the small intestine (duodenum). Symptoms you might have:
- Nausea
- Weight loss
- Loss of appetite
- Vomiting (if narrow segments of bowel are obstructed)
Jejunoileitis: Inflames the middle part of the small intestine (jejunum). Symptoms you may have:
- Cramps after meals
- Fistulas
- Diarrhea
- Abdominal pain that can become intense.
Crohn's (granulomatous) colitis: Inflames only the colon. Symptoms you may have:
- Skin lesions
- Joint pain
- Diarrhea
- Rectal bleeding
- Ulcers, fistulas, and abscesses around the anus
Perianal Crohn's disease (PCD): ): Is a common type of Crohn's disease that causes inflammation around the anus. It can cause tags, fissures, fistulae, abscesses, or stenosis. Symptoms include:
- Pain
- Itching
- Bleeding
- Purulent discharge
- Incontinence of stool
There can be an overlap between these types of Crohn's disease. Sometimes, more than one area of your digestive tract is affected. The disease can be further divided by phenotypes, or physical traits, as it gets worse.
For Crohn’s, these are based on:
Your age when you were diagnosed:
- Child
- Young adult
- Elderly
The affected body part:
- Terminal ileum
- Colon
- Ileocolon
- Upper gastrointestinal tract
How the disease behaves:
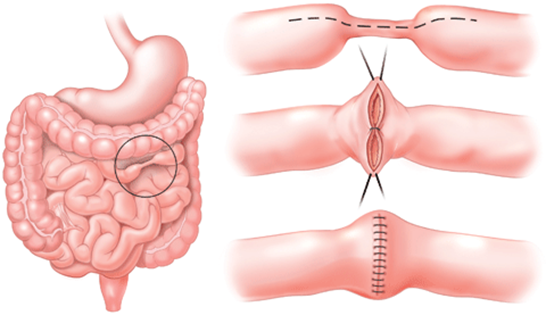 Stricturing: The disease causes swelling and scarring on the walls of your intestine. This makes the walls thicker and can form strictures, or narrowed areas, that lead to blockages.
Stricturing: The disease causes swelling and scarring on the walls of your intestine. This makes the walls thicker and can form strictures, or narrowed areas, that lead to blockages.- Penetrating: Crohn’s causes fistulas, perianal ulcers, inflammatory masses, or abscesses.
- Uncomplicated
There are three types of Ulcerative Colitis, each with their own set of symptoms.6
Ulcerative Proctitis - In ulcerative proctitis, bowel inflammation is limited to the rectum. This condition typically affects less than six inches of the rectum, and it is not associated with an increased risk of cancer. Symptoms may include:
- Rectal bleeding
- Rectal pain
- Urgency in your bowel movements
Left-Sided Colitis - In this form of ulcerative colitis, continuous inflammation begins at the rectum and extends as far into the colon as the splenic flexure, which is a bend in the colon near the spleen. Left-sided colitis also includes proctosigmoiditis, which affects rectum and the lower segment of colon located right above the rectum known as the sigmoid colon. Symptoms may include:
- Loss of appetite
- Weight loss
- Bloody diarrhea
- Pain on the left side of the abdomen
 Extensive Colitis - This type of ulcerative colitis affects the entire colon. Continuous inflammation begins at the rectum and extends beyond the splenic flexure. Symptoms may include:
Extensive Colitis - This type of ulcerative colitis affects the entire colon. Continuous inflammation begins at the rectum and extends beyond the splenic flexure. Symptoms may include:
- Loss of appetite
- Bloody diarrhea
- Abdominal pain
- Weight loss
Traditional Medical Treatment for Crohn’s and Colitis
There is currently no cure for Crohn's disease, and there is no single treatment that works for everyone.
One goal of medical treatment is to reduce the inflammation that triggers your signs and symptoms. Another goal is to improve long-term prognosis by limiting complications. In the best cases, this may lead not only to symptom relief but also to long-term remission.
Anti-Inflammatory Drugs -Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. They include:
- Corticosteroids. Corticosteroids such as prednisone and budesonide (Entocort EC) can help reduce inflammation in your body, but they don't work for everyone with Crohn's disease. Corticosteroids may be used for short-term (3 to 4 months) symptom improvement and to induce remission. Corticosteroids may also be used in combination with an immune system suppressor to induce the benefit from other medications. They are then eventually tapered off.
- Oral 5-aminosalicylates. These drugs are generally not beneficial in Crohn's disease. They include sulfasalazine (Azulfidine), which contains sulfa, and mesalamine (Delzicol, Pentasa, others). Oral 5-aminosalicylates were widely used in the past but now are generally considered of very limited benefit.
Immune System Suppressors - These drugs also reduce inflammation, but they target your immune system, which produces the substances that cause inflammation. For some people, a combination of these drugs works better than one drug alone. Immune system suppressors include:
 Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are the most widely used immunosuppressants for treatment of inflammatory bowel disease. Taking them requires that you follow up closely with your doctor and have your blood checked regularly to look for side effects, such as a lowered resistance to infection and inflammation of the liver. They may also cause nausea and vomiting.
Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are the most widely used immunosuppressants for treatment of inflammatory bowel disease. Taking them requires that you follow up closely with your doctor and have your blood checked regularly to look for side effects, such as a lowered resistance to infection and inflammation of the liver. They may also cause nausea and vomiting.- Methotrexate (Trexall). This drug is sometimes used for people with Crohn's disease who don't respond well to other medications. You will need to be followed closely for side effects.
Biologics -This class of therapies targets proteins made by the immune system. Types of biologics used to treat Crohn's disease include:
- Vedolizumab (Entyvio). This drug works by stopping certain immune cell molecules — integrins — from binding to other cells in your intestinal lining. Vedolizumab is a gut-specific agent and is approved for Crohn's disease. A similar medication to vedolizumab known as natalizumab was previously used for Crohn's disease but is no longer used due to side effect concerns, including a fatal brain disease.
- Infliximab (Remicade), adalimumab (Humira) and certolizumab pegol (Cimzia). Also known as TNF inhibitors, these drugs work by neutralizing an immune system protein known as tumor necrosis factor (TNF).
- Ustekinumab (Stelara). This was recently approved to treat Crohn's disease by interfering with the action of an interleukin, which is a protein involved in inflammation.
- Risankizumab (Skyrizi).This medication acts against a molecule known as interleukin-23 and was recently approved for treatment of Crohn's disease.
Antibiotics - Antibiotics can reduce the amount of drainage from fistulas and abscesses and sometimes heal them in people with Crohn's disease. Some researchers also think that antibiotics help reduce harmful bacteria that may be causing inflammation in the intestine. Frequently prescribed antibiotics include ciprofloxacin (Cipro) and metronidazole (Flagyl).
Other Medications - In addition to controlling inflammation, some medications may help relieve your signs and symptoms. But always talk to your doctor before taking any nonprescription medications. Depending on the severity of your Crohn's disease, your doctor may recommend one or more of the following:
 Anti-diarrheals. A fiber supplement, such as psyllium powder (Metamucil) or methylcellulose (Citrucel), can help relieve mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide (Imodium A-D) may be effective. These medications could be ineffective or even harmful in some people with strictures or certain infections. Please consult your health care provider before you take these medications.
Anti-diarrheals. A fiber supplement, such as psyllium powder (Metamucil) or methylcellulose (Citrucel), can help relieve mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide (Imodium A-D) may be effective. These medications could be ineffective or even harmful in some people with strictures or certain infections. Please consult your health care provider before you take these medications.- Pain relievers. For mild pain, your doctor may recommend acetaminophen (Tylenol, others) — but not other common pain relievers, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). These drugs are likely to make your symptoms worse and can make your disease worse as well.
- Vitamins and supplements. If you're not absorbing enough nutrients, your doctor may recommend vitamins and nutritional supplements.
Nutrition Therapy - Your doctor may recommend a special diet given by mouth or a feeding tube (enteral nutrition) or nutrients infused into a vein (parenteral nutrition) if you have Crohn's disease. This can improve your overall nutrition and allow the bowel to rest. Bowel rest may reduce inflammation in the short term.
Your doctor may use nutrition therapy short term and combine it with medications, such as immune system suppressors. Enteral and parenteral nutrition are typically used to get people healthier prior to surgery or when other medications fail to control symptoms.
Your doctor may also recommend a low residue or low-fiber diet to reduce the risk of intestinal blockage if you have a narrowed bowel (stricture). A low residue diet is designed to reduce the size and number of your stools.
Surgery -If diet and lifestyle changes, drug therapy, or other treatments don't relieve your signs and symptoms, your doctor may recommend surgery. Nearly half of those with Crohn's disease will require at least one surgery. However, surgery does not cure Crohn's disease.
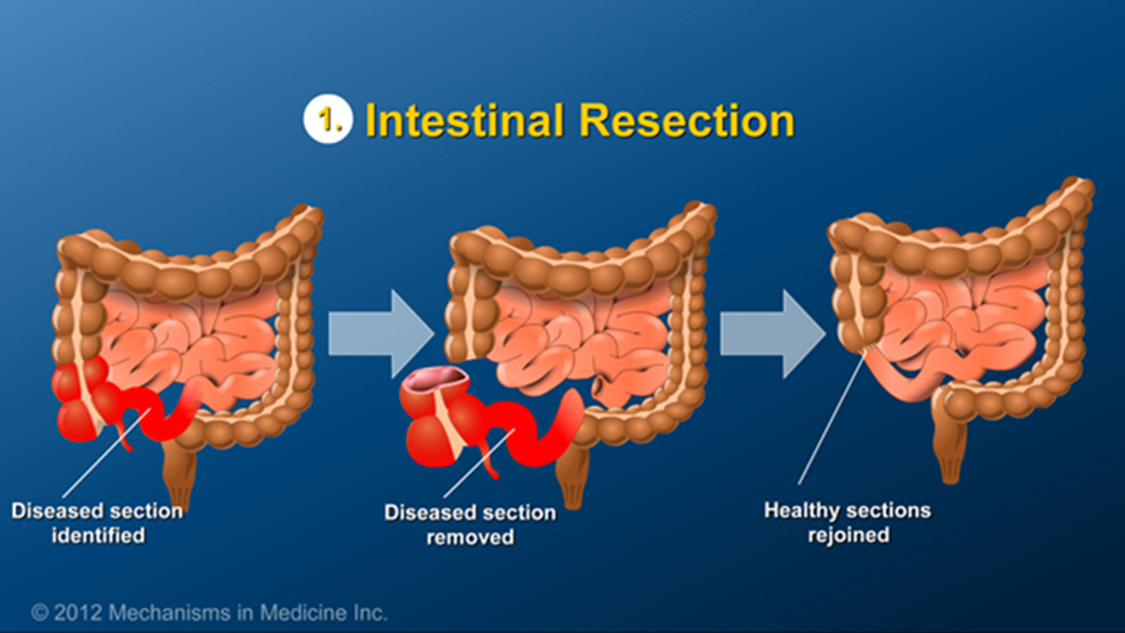
During surgery, your surgeon removes a damaged portion of your digestive tract and then reconnects the healthy sections. Surgery may also be used to close fistulas and drain abscesses. The benefits of surgery for Crohn's disease are usually temporary. The disease often recurs, frequently near the reconnected tissue. The best approach is to follow surgery with medication to minimize the risk of recurrence.
Ulcerative Colitis treatment usually involves either medication therapy or surgery. Several categories of medications may be effective in treating Ulcerative Colitis. The type you take will depend on the severity of your condition. The medications that work well for some people may not work for others. It may take time to find a medication that helps you. In addition, because some medications have serious side effects, you'll need to weigh the benefits and risks of any treatment.7
Anti-Inflammatory Medications - Anti-inflammatory medications are often the first step in the treatment of Ulcerative Colitis and are appropriate for most people with this condition. These include:
- 5-aminosalicylates. Examples of this type of medication include sulfasalazine (Azulfidine), mesalamine (Delzicol, Rowasa, others), balsalazide (Colazal) and olsalazine (Dipentum). Which medication you take and how you take it — by mouth or as an enema or suppository — depends on the area of your colon that's affected.
- Corticosteroids.These medications, which include prednisone and budesonide, are generally reserved for moderate to severe Ulcerative Colitis that doesn't respond to other treatments. Corticosteroids suppress the immune system. Due to the side effects, they are not usually given long term.
Immune System Suppressors - These medications also reduce inflammation, but they do so by suppressing the immune system response that starts the process of inflammation. For some people, a combination of these medications works better than one medication alone. Immunosuppressant medications include:
 Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are commonly used immunosuppressants for the treatment of inflammatory bowel disease. They are often used in combination with medications known as biologics. Taking them requires that you follow up closely with your provider and have your blood checked regularly to look for side effects, including effects on the liver and pancreas.
Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are commonly used immunosuppressants for the treatment of inflammatory bowel disease. They are often used in combination with medications known as biologics. Taking them requires that you follow up closely with your provider and have your blood checked regularly to look for side effects, including effects on the liver and pancreas.- Cyclosporine (Gengraf, Neoral, Sandimmune). This medication is typically reserved for people who haven't responded well to other medications. Cyclosporine has the potential for serious side effects and is not for long-term use.
- "Small molecule" medications.More recently, orally delivered agents, also known as "small molecules," have become available for IBD treatment. These include tofacitinib (Xeljanz), upadacitinib (Rinvoq) and ozanimod (Zeposia). These medications may be effective when other therapies don't work. Main side effects include the increased risk of shingles infection and blood clots. The U.S. Food and Drug Administration (FDA) recently issued a warning about tofacitinib, stating that preliminary studies show an increased risk of serious heart-related problems and cancer from taking this medication. If you're taking tofacitinib for Ulcerative Colitis, don't stop taking it without first talking with your health care provider.
Biologics -This class of therapies targets proteins made by the immune system. Types of biologics used to treat Ulcerative Colitis include:
- Infliximab (Remicade), adalimumab (Humira) and golimumab (Simponi). These medications, called tumor necrosis factor (TNF) inhibitors, work by neutralizing a protein produced by your immune system. They are for people with severe Ulcerative Colitis who don't respond to or can't tolerate other treatments. TNF inhibitors are also called biologics.
- Vedolizumab (Entyvio). This medication is approved for treatment of Ulcerative Colitis for people who don't respond to or can't tolerate other treatments. It works by blocking inflammatory cells from getting to the site of inflammation.
- Ustekinumab (Stelara). This medication is approved for treatment of Ulcerative Colitis for people who don't respond to or can't tolerate other treatments. It works by blocking a different protein that causes inflammation.
Other Medications - You may need additional medications to manage specific symptoms of Ulcerative Colitis. Always talk with your health care provider before using over-the-counter medications. Your provider may recommend one or more of the following.
- Anti-diarrheal medications.For severe diarrhea, loperamide (Imodium A-D) may be effective. If you have Ulcerative Colitis, do not take anti-diarrheal medications without first talking with your health care provider. These medications may increase the risk of an enlarged colon (toxic megacolon).
- Pain relievers. For mild pain, your provider may recommend acetaminophen (Tylenol, others) — but not ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium, which can worsen symptoms and increase the severity of disease.
- Antispasmodics. Sometimes health care providers will prescribe antispasmodic therapies to help with cramps.
- Iron supplements. If you have chronic intestinal bleeding, you may develop iron deficiency anemia and be given iron supplements.
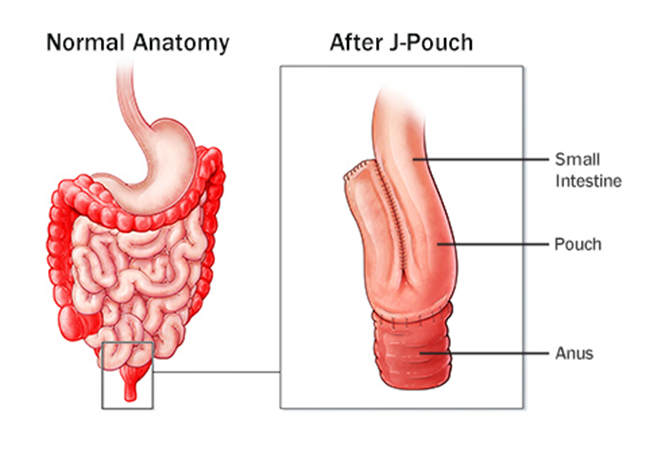 Surgery -Surgery can eliminate Ulcerative Colitis and involves removing your entire colon and rectum (proctocolectomy). In most cases, this involves a procedure called ileoanal anastomosis (J-pouch) surgery. This procedure eliminates the need to wear a bag to collect stool. Your surgeon constructs a pouch from the end of your small intestine. The pouch is then attached directly to your anus, allowing you to expel waste in the usual way. This surgery may require 2 to 3 steps to complete.
Surgery -Surgery can eliminate Ulcerative Colitis and involves removing your entire colon and rectum (proctocolectomy). In most cases, this involves a procedure called ileoanal anastomosis (J-pouch) surgery. This procedure eliminates the need to wear a bag to collect stool. Your surgeon constructs a pouch from the end of your small intestine. The pouch is then attached directly to your anus, allowing you to expel waste in the usual way. This surgery may require 2 to 3 steps to complete.
Cancer Surveillance - You will need more-frequent screening for colon cancer because of your increased risk. The recommended schedule will depend on the location of your disease and how long you have had it. People with inflammation of the rectum, also known as proctitis, are not at increased risk of colon cancer.
If your disease involves more than your rectum, you will require a surveillance colonoscopy every 1 to 2 years. This begins as soon as eight years after diagnosis if the majority of colon is involved. Or 15 years after diagnosis if only the left side of your colon is involved.
Complications of Crohn’s and Colitis
In addition to the signs and symptoms of IBD described on the preceding pages, some people develop complications that may require urgent medical care.
Complications of Crohn’s disease include:
- Fistula—ulcers on the wall of the intestine that extend and cause a tunnel (fistula) to another part of the intestine, the skin or another organ.
- Stricture—a narrowing of a section of intestine caused by scarring, which can lead to an intestinal blockage.
- Abscess—a collection of pus, which can develop in the abdomen, pelvis, or around the anal area.
- Perforated bowel—chronic inflammation of the intestine may weaken the wall to such an extent that a hole develops.
- Malabsorption and malnutrition, including deficiency of vitamins and minerals.
 Complications of Ulcerative Colitis include:
Complications of Ulcerative Colitis include:
- Heavy, persistent diarrhea, rectal bleeding, and pain.
- Perforated bowel—chronic inflammation of the intestine may weaken the intestinal wall to such an extent that a hole develops.
- Toxic megacolon—severe inflammation that leads to rapid enlargement of the colon.
Complications Outside the GI Tract:
Not all complications of IBD are confined to the GI tract. For reasons that are not entirely understood, some people develop symptoms that are related to the disease but affect other parts of the body. The most common of these complications affect the skin and bones. These extraintestinal complications may be evident in the:
- Eyes (redness, pain, and itchiness)
- Mouth (sores)
- Joints (swelling and pain)
- Skin (tender bumps, painful ulcerations, and other sores/rashes)
- Bones (osteoporosis)
- Kidney (stones)
- Liver (primary sclerosing cholangitis, hepatitis, and cirrhosis)—occurs rarely
Long-Term Side Effects of Crohn’s and Colitis Medicines
If you’ve been diagnosed with Crohn’s or Colitis and your plan is to just take meds for the rest of your life, you need to know there are long term side effects to this strategy. Below is a list of the common medicines patients are put on when they are diagnosed with Crohn’s or Colitis along with the potential side effects of those medicines.
5-ASAs
These medications are also known as aminosalicylates. They lower inflammation in your digestive tract. They’re best for mild to moderate flares and can help you avoid relapses (when your symptoms come back). They usually come in tablets. But they’re also given rectally as an enema or suppository. Examples of 5-ASAs are:
- Balsalazide (Colazal)
- Mesalamine (Asacol HD, Delzicol)
- Sulfasalazine (Azulfidine)
Side effects are most common with sulfasalazine. They include:
- Nausea
- Headache
- Fever
- Rash
- Male infertility that can be reversed
When you first start this drug, you might also have:
- Appetite loss
- Sunlight sensitivity
- Nervousness
It’s rare, but sulfasalazine could also cause inflammation of your pancreas. Other uncommon symptoms include:
- An inflamed liver, kidney, or lung
- Stevens-Johnson syndrome, a serious allergic reaction
- Hemolysis, a disorder where red blood cells are destroyed faster than your body can make them
Other 5-ASA drugs generally have fewer side effects, compared to sulfasalazine. Common ones include:
 Headache
Headache- A feeling of sickness
- Gas
- Cramps
- Less common side effects include:
- Skin rash
- Hair loss
- Worsened inflammation in your colon
Rarely, these drugs can cause inflammation in your lung, pancreas, kidney, or the tissue around your heart.9
Corticosteroids
These anti-inflammatory drugs suppress your immune system. This means they keep your immune system from working the way it should. Corticosteroids are typically used to treat moderate to severe UC. You can take them orally or rectally. They can cause short- and long-term side effects, so you shouldn’t take them regularly. Types of corticosteroids include:
- Budesonide
- Hydrocortisone
- Methylprednisolone
- Prednisone
Because they suppress your immune system, corticosteroids can lead to infections. These include:
- Yeast infection in the mouth
- Yeast infection in female sex organs
- Urinary tract infections (UTIs)
Side effects that usually go away after you stop corticosteroids include:
- High blood pressure
- High blood sugar
- Weight gain
- Stretch marks
- Acne
- Growth interruption in kids
- More facial hair
- Trouble sleeping
- Mood swings
- Psychosis and other psychiatric symptoms
You could also get cataracts or osteoporosis (weakening of your bones). But they won’t just go away after you stop taking corticosteroids. Your doctor will have to treat these conditions.
Immunomodulators
These medications also suppress your immune system so it can’t cause more inflammation. They include:
- Azathioprine (Azasan, Imuran)
- Mercaptopurine (Purinethol, Purixan)
- Cyclosporine (Gengraf, Neoral, Sandimmune)
- Methotrexate paired with folic acid
Side effects of these drugs include:
- Nausea
- Headaches
- Diarrhea
- General feeling of sickness
- Canker sores
- Rash
- Fever
- Joint pain
- Liver inflammation
- Lowered kidney function
- Hepatitis
- Higher risk of infection
- Diabetes
- High cholesterol
- Sleep issues or fatigue
- Seizure
- High blood pressure
- Tingling in your fingers and feet
- More facial hair
- Low white blood cell count
 Rare side effects include:
Rare side effects include:
- Inflammation of the pancreas or lung
- Bone marrow suppression (when fewer blood cells are made in your bone marrow)
- Higher risk of lymphoma
- Scarring of your liver
Biologics
These medications are best for moderate to severe UC. They’re antibodies that stop certain proteins from causing inflammation. Biologics are made from natural substances. Examples include:
- Adalimumab (Humira)
- Golimumab (Simponi)
- Infliximab (Remicade)
- Ustekinumab (Stelara)
- Vedolizumab (Entyvio)
People who take biologics and have a history of hepatitis B could trigger the condition. So, it’s important to get a blood test before starting these medications.
Other common side effects can include:
- A higher chance of infection
- Shortness of breath
- Chills
- Itchiness
- Redness
- Eye or lip itchiness
- Full body sensitivity or rash
Less common symptoms are:
- Sudden vision issues
- Numbness or tingling
- Swollen ankles or hands
- Shortness of breath
- Heart failure
- Lupus-like syndrome, which includes a rash across your face and arms that gets worse in the sun or new joint and body pain
JAK Inhibitors
JAK inhibitors, or Janus kinase inhibitors, suppress your immune system to block the JAK enzyme. This stops inflammation. You’ll take the JAK inhibitor tofacitinib (Xeljanz) by mouth to treat moderate to severe UC.
If you notice any side effects besides diarrhea, you should call your doctor right away. These can include:
 Black poop
Black poop- Bloody or cloudy pee
- A hard time peeing, painful/burning feeling while peeing, or frequently having to pee
- Pain in your bladder
- Blurry vision
- Aches or pains
- Chest tightness, pain, or a hard time breathing
- Cough
- Chills
- Fever
- Dizziness
- Ear congestion or pounding in your ears
- Headache
- Sensitive skin
- Loss of voice
- Pain in your lower side or back
- Nervousness
- Slower or faster heartbeat
- Sneezing
- Sore throat
- Stuffy/runny nose
- Swollen glands
- Fatigue or weakness
- Weight loss
- Yellow skin or eyes
What Traditional Medicine is Not Telling You About Crohn’s and Colitis
The information I am about to share with you was not taught to me during any of my medical training. What medical school, internship, internal medicine residency, and my Gastroenterology fellowship taught me was how to diagnose symptoms, prescribe medicines and do amazing colonoscopies and upper endoscopies. What it didn’t teach was the true reason why people are having symptoms to begin with.
There are many treatments for Crohn’s and Colitis and although they might be helping people get to and stay in remission, they are not addressing the issues caused by the disease. The “other
medicines” patients are put on to deal with the symptoms of Crohn’s and Colitis (such as antidiarrhea or pain meds) are just band aids, they are not actually fixing the problem. The way I see it, although Crohn’s and Colitis is most likely a hereditary disease, it can also be caused by four key issues in the body:
 1. Nutrient and water absorption issues.
1. Nutrient and water absorption issues. - 2. Microbiome / gut bacteria issues.
- 3. Toxicity build-up / inflammation issues.
- 4. Poor diet / lack of good nutrition issues.
When all four of these occur, it is a recipe for disaster in the gut causing tons of inflammation. And like I said, although there are medicines to stop inflammation receptors, it’s not fixing the problem. If someone is diagnosed with Crohn’s and Colitis, we need to help support the body and fix these four key issues before any true healing is going to happen. To do this, we need to start addressing the following:
- 1. The importance behind digesting and absorbing food properly and the tools to do it.
- 2. The importance of drinking water and that not all water is created equal.
- 3. The importance of good healthy gut bacteria and the tools to replenish it on a regular basis.
- 4. The best way to gently detoxify the body and keep it clean on a day-to-day basis.
- 5. The reason why eating green is so important and how to get people off the Standard American Diet (SAD).
The next sections of this e-book are going to go into major detail on these five topics and why in addition to the IBD medicines available today, these five actions are the key to turning around Crohn’s and Colitis for good.
Why It’s Important to Digest Your Food Properly
When you eat food, it goes into your stomach as a solid. Obviously, we chew it, but we don’t chew it into a liquid. Your body cannot use food in a solid form, it must be broken down into a liquid for your body to benefit from it. This means when you eat, your body is supposed to go to work for you – making enzymes and acid. There is a different enzyme produced to digest all different types of foods:
- • Amylase & Diastase - break down starch into sugars / glucose.
- • Protease- breaks down protein into amino acids.
- • Lipase- breaks down fat into fatty acids.
- • Invertase - breaks sugar down into glucose and fructose.
- • Lactase - breaks down sugar found in dairy products.
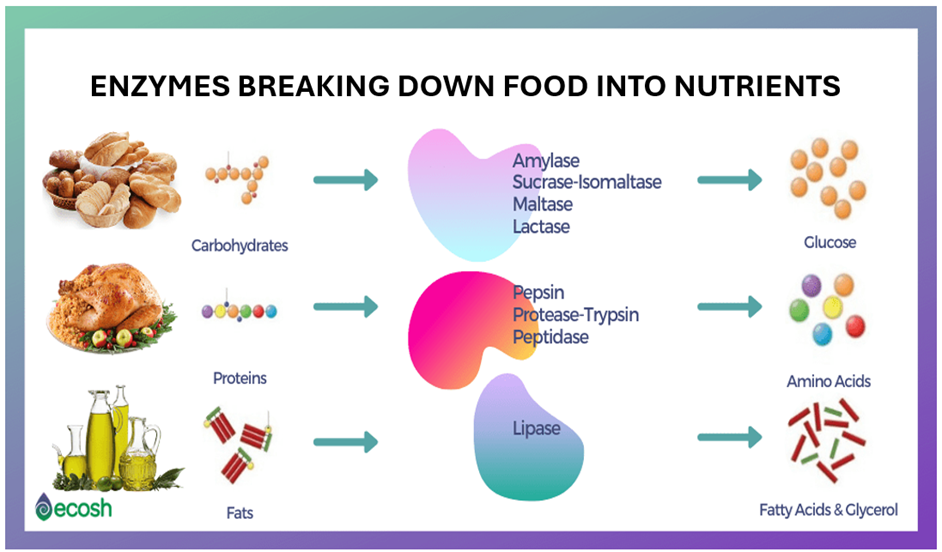
The acid that gets produced in the stomach helps to digest protein in addition to killing off germs, viruses or bugs found on our food. Our food is not sterile, so the acid helps to protect us from all the items we consume that the body shouldn’t be exposed to. Producing the appropriate amount of enzymes and acid is a crucial step in the digestive process. For your food to be absorbed and assimilated into the body the food must be broken down properly. If you are lacking enzymes or acid your food will sit around too long in the stomach causing lots of digestive issues but in addition to that you will not be able to benefit from the food itself.
Imagine this – even if you are eating the healthiest diet in the world, if your body is not breaking it down properly, you are not benefiting from what you are eating. This can cause you to be tired, have low energy, have a foggy brain, etc. Anyone out there experiencing any of these symptoms?
In addition, if you are not getting vitamins and minerals from the food you are eating, the body is very smart. It knows you need vitamins and minerals to function and so guess what it does, it starts to rob from itself. And the first place it goes is the bone and the muscle because that is where we have the most vitamins and minerals stored up.
Digesting your food properly is the first step to not only eliminating digestive issues but getting you off of over-the-counter and prescription meds while at the same time giving you your life back. Knowing that one of the key issues with Crohn’s and Colitis patients is the importance of digesting and absorbing food properly, you can see how important taking a good digestive enzyme on a daily basis can be.
Why Hydrating Properly is So Important
The most important thing you can do for your body daily is to drink water. The only thing that hydrates the body is water – everything else dehydrates the body (juices, caffeinated drinks, energy drinks, sodas, lemonade, iced tea, alcohol, etc.) Just to replenish what you lose daily; you need to drink half of your body weight in ounces of water per day. This means if you weigh 200 lbs. you should be drinking 100 ounces of water per day. And if you drink that cup of coffee or two every day (which is caffeine, which is a diarrhetic so it’s going to make you urinate), you need even more water to compensate. Most people do not drink the recommended amount of water every day and wonder why they don’t feel good. Out of all the advice we’ve given patients over the years, this is the one piece of advice patients have mentioned that made the biggest impact on them – that was to drink more water. The more water you drink and the less of everything else you drink, the healthier the body is going to be.
Not only does drinking water keep the body hydrated but it is also the best way to detoxify the body – washing away the toxic build up. And if you want to take your water drinking to the next level you need to consider drinking alkaline water. Especially if you’re the type of person who doesn’t drink a lot of water because it makes you pee a lot. Alkaline water will absorb deeper into the body, detoxing you better and hopefully causing you to pee less often. To learn what alkaline water is and how it works be sure to check out the next section on my approach to Crohn’s and Colitis.
 Finally, let’s discuss water additives, especially electrolytes. The big thing in the last couple of years are flavored powders or liquids that can be added to water to give it some taste while at the same time adding some extra vitamins, minerals and sometimes energy boosters to the body. People may use these because they feel water doesn’t have a taste, or they think it’s boring to drink water, or maybe they are trying to supplement something in the diet or give themselves that extra boost they feel they need to get through the day. Let me be clear, most of the powders and liquids on the market today are loaded with chemicals, artificial flavors, artificial sugars and preservatives. Even the ones that say no sugar added, nine times out of ten they will have artificial sugar which is worse for you than regular sugar. I guarantee these are only contributing to your problem, not solving it.
Finally, let’s discuss water additives, especially electrolytes. The big thing in the last couple of years are flavored powders or liquids that can be added to water to give it some taste while at the same time adding some extra vitamins, minerals and sometimes energy boosters to the body. People may use these because they feel water doesn’t have a taste, or they think it’s boring to drink water, or maybe they are trying to supplement something in the diet or give themselves that extra boost they feel they need to get through the day. Let me be clear, most of the powders and liquids on the market today are loaded with chemicals, artificial flavors, artificial sugars and preservatives. Even the ones that say no sugar added, nine times out of ten they will have artificial sugar which is worse for you than regular sugar. I guarantee these are only contributing to your problem, not solving it.
The thing you do need is electrolytes. Electrolytes are salts that are responsible for keeping the body properly hydrated so the muscles and nerves can function properly. The human body is composed mostly of salt water. Have you ever tasted your sweat or your tears? They are salty! Your body is a giant saltwater bag and all day long you are losing salt water, when you urinate, when you sweat or when you talk. If you do not replace this salt water your body becomes very dehydrated (again, a key symptom of Crohn’s and Colitis). Most people who are drinking water are not drinking water with electrolytes. Some might be drinking things like Gatorade, Powerade, etc. but again those drinks are loaded with chemicals, sugar, artificial sugar, preservatives, and dyes. The bottom line, they are not helping the body but hurting it. There is a solution for a good pure, clean, electrolyte powder to use in your water. The next section on my approach will explain it in further detail.
And if you still think water doesn’t taste good, consider adding fresh vegetables or fruit to your water. This is a natural way of flavoring your water without needing store bought products that will add toxicity to the body. Some ideas include lemon, lime, cucumber, watermelon, blueberries, strawberries, etc.
The Importance of Good Healthy Gut Bacteria
Your digestive system is home to trillions of microorganisms, creating an ecosystem called the “gut flora.” Probiotics are the good bacteria, which are needed to create a balance throughout the body.
The body has both good and bad bacteria. The word “probiotic” literally means “good life,” which is fitting since it has been proven to treat many uncomfortable symptoms. For women, an imbalance of bacteria in the vaginal area may lead to a yeast infection. If there is an imbalance of bacteria in the urethra, a urinary tract infection may develop. The gut also needs to have a balance of bacteria, or else diarrhea, constipation, gas, and bloating may be experienced, all common symptoms of someone suffering from Crohn’s or Colitis.
Imbalances of flora in the body may occur for many different reasons. Some common culprits for throwing it off balances include:
- • Aging
- • Eating a nutritionally depleted diet
- • Stress
- • Alcohol consumption
- • Smoking
- • Steroids
- • Birth control pills
- • Antibiotics; keep in mind that a large amount of meat and dairy consumed today have been treated with antibiotics, which affect our flora
- • Chemicals in food, soaps, lotions and perfumes
- • Diabetes; sugar provides food for bad bacteria
Probiotics are needed to fulfil many functions. They act as a barrier to protect us against invaders in the body; bad bacteria, parasites, fungi, viruses, toxins etc.
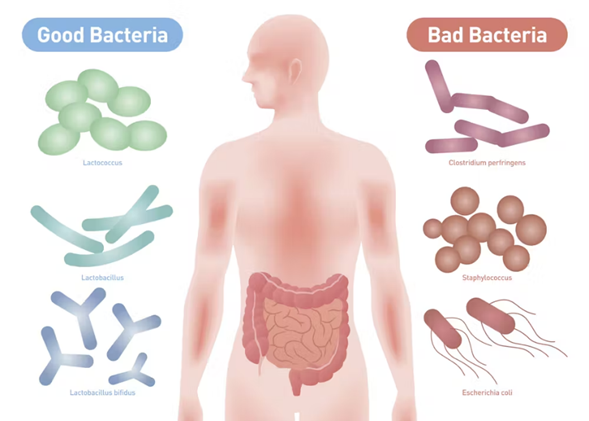 On a daily basis, we unconsciously consume various microbes that could potentially cause sickness. In a body that has plenty of “good bacteria,” these microbes will pass with no negative effects. However, if bad microbes are ingested in a body with an imbalanced gut flora, these microbes will cause sickness. The “bad bacteria” that are constantly in our system, are kept under control by the “good bacteria.” If the good bacterium becomes imbalanced, “bad bacteria” is given an opportunity to break through the gut walls and invade other parts of the body.
On a daily basis, we unconsciously consume various microbes that could potentially cause sickness. In a body that has plenty of “good bacteria,” these microbes will pass with no negative effects. However, if bad microbes are ingested in a body with an imbalanced gut flora, these microbes will cause sickness. The “bad bacteria” that are constantly in our system, are kept under control by the “good bacteria.” If the good bacterium becomes imbalanced, “bad bacteria” is given an opportunity to break through the gut walls and invade other parts of the body.
More than half of our immune system is located in the gut wall, so it is vital to keep that part of our body healthy. Many illnesses can be linked back to abnormal gut flora. In addition to aiding our immune system, probiotics support digestion. They aid in producing enzymes, which help to break down food, and transport vitamins, minerals, and other nutrients. Several nutrients cannot survive in the body if they are not quickly absorbed, so without a healthy gut flora, nutrient deficiency is likely. Crohn’s and Colitis have been directly linked to poor gut flora. Taking a good healthy probiotic every day is critical to those suffering from this diagnosis. It will help keep the gut flora strong allowing for healthy digestion and an immune system that can work hard to keep the body well.
Why it’s Important to Detoxify Your Body
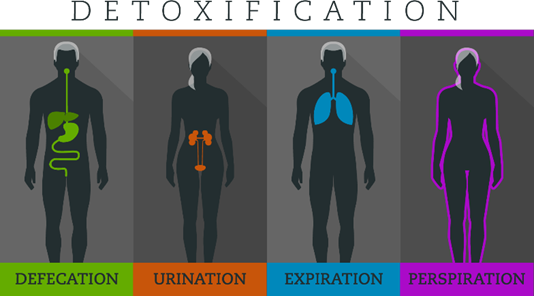 If you had asked me 15 years ago about the importance of detoxing the body, I would have referred you to a naturopathic doctor, but today it is my favorite topic to discuss. As a Gastroenterologist one of my favorite organs (the colon) is responsible for much of that detoxification. Our body has many natural mechanisms for detoxing, for example urine, stool, sweat, and breath. As we age, our body slows down, and we aren’t detoxing like we should. Over time, as our body slows down, we hold on to more of these toxins making us experience aches and pains.
If you had asked me 15 years ago about the importance of detoxing the body, I would have referred you to a naturopathic doctor, but today it is my favorite topic to discuss. As a Gastroenterologist one of my favorite organs (the colon) is responsible for much of that detoxification. Our body has many natural mechanisms for detoxing, for example urine, stool, sweat, and breath. As we age, our body slows down, and we aren’t detoxing like we should. Over time, as our body slows down, we hold on to more of these toxins making us experience aches and pains.
I have patients in their early 20’s that are experiencing these issues because this is a generation of kids of that have lived off processed foods, fast foods, energy drinks, fancy coffees, recreational drugs, vapes, etc. Imagine the toxins their bodies take in every day and even though they are young, their body can’t keep up.
Our body is a healing vessel, it wants us to be well, but when we continue to expose it to toxins day in and day out, it can only do so much. At some point it’s going to throw up its hands and say, “enough is enough, you’re on your own!” This is when symptoms like aches, pains, tiredness, low energy, foggy brain, set in. And unfortunately, when this happens the pharmaceutical and food industry will tell us to take pain meds or drink more caffeine. I have several friends that haven’t been to their doctor in decades because they say they “feel fine” yet are drinking energy drinks and taking pain meds every day for one reason or another. In the end, adding more toxicity to the body - it truly is an endless cycle. The more toxic the body, the greater the inflammation, the greater the inflammation the higher likelihood of IBD.
The bottom line is, we are all moving in the same direction, it just depends on how fast you want to get there. Keeping a clean body is one way to slow the process of aging, it can also help you get off unnecessary prescription and over the counter medicines and most importantly reverse those aches and pains. Most importantly, keeping a clean body will reduce inflammation and minimize IBD symptoms and flares.
Why Eating Greens is So Important
Your body needs vitamins and minerals from green vegetables to build healthy red blood. Healthy red blood builds healthy tissue, which builds healthy organs which builds a healthy body. Without healthy vitamins and minerals being consumed on a regular basis your body will not only struggle with making healthy red blood but it will also struggle with detoxification, and normal bodily functions. Your body wants to get vitamins and minerals from real food, not synthetic capsules (supplements made in a lab). Many of my patients are taking numerous supplements every day for various reasons – vitamin and mineral deficiencies, issues with skin, hair, nails, anemia, etc. I have many patients that are taking 15 plus supplements every day and they wonder why they have stomach pain. Your body doesn’t know what to do with all those capsules. And most supplements today are loaded with fillers (that can cause issues in the body – especially digestive issues). Supplement manufacturers add fillers because it makes them more affordable to make; therefore, increasing their profits.
 The best thing you can do for your body is to eat a variety of greens. When I ask patients if they eat vegetables, the most common vegetables I hear are corn, carrots, and peas. Corn and carrots are not green, and peas are more of a starch than a vegetable. On the flip side, a patient will tell me they eat a spinach salad every day. Although spinach is good for you, every vegetable, and every fruit for that matter, has its own vitamin and mineral makeup. Spinach has its own vitamins and minerals; broccoli has its own, etc. When you eat spinach every day, you’re only giving your body the vitamins and minerals from spinach. Over time, the body says, “oh no, not spinach again.”
The best thing you can do for your body is to eat a variety of greens. When I ask patients if they eat vegetables, the most common vegetables I hear are corn, carrots, and peas. Corn and carrots are not green, and peas are more of a starch than a vegetable. On the flip side, a patient will tell me they eat a spinach salad every day. Although spinach is good for you, every vegetable, and every fruit for that matter, has its own vitamin and mineral makeup. Spinach has its own vitamins and minerals; broccoli has its own, etc. When you eat spinach every day, you’re only giving your body the vitamins and minerals from spinach. Over time, the body says, “oh no, not spinach again.”
This is why mixing up your greens is so important. Examples of green vegetables include broccoli, asparagus, Brussel sprouts, green beans, okra, leaks, avocados, micro greens, peppers, zucchini, chard, collard greens, Bok choy, kale, turnip greens, romaine, spring mix, butter lettuce, spinach, red leaf lettuce, green leaf lettuce, arugula, cucumbers, celery, watercress, and cabbage just to name a few. Eating fresh vegetables instead of canned or frozen is also important. Anytime a vegetable is frozen or canned it loses some of its nutritional value.
Many of my patients have told me they don’t like eating greens, if that is the case, you must supplement them. But supplement with a green powder that contains real food – more on this below. Other patients tell me they stopped eating green because it doesn’t agree with them anymore. If this is the case, you need to read the e-book on Acid Reflux to learn why you’re not digesting them well anymore and what you can do about it. The bottom line, if you want to minimize IBD flares, you must be consuming greens daily in one way or another.
A Different Approach to Crohn’s and Colitis
In 2007, I approached my wife and Office Manager Tina and told her how frustrated I was with medicine. I was running all the tests, doing all the procedures, and prescribing all the medicines and could not figure out why my patients were still hurting. That frustration led us on a two-year journey to learn what my medical degree did not teach me about the body and how it works, in addition to what is happening in the medical industry, pharmaceutical industry and food industry to cause so many health problems in our society.
After we learned what we did, we felt obligated to share this with our patients and we’ve been doing so since 2010. Tina was so passionate about what we learned, she went back to school and received her Certificate in Holistic Nutrition so she could help me deliver this message to as many people as we possibly could. Since we started on this journey, we have helped tens of thousands of patients and wellness clients eliminate their symptoms naturally, helping their bodies work again like they were meant to work. And the best part of it all, is it’s not as hard as you may think to turn it all around, no matter how long you’ve been suffering or how old you are. If you are willing to put in the time, effort and invest in yourself, you can have your life back too.
IBD is so prevalent today but the great thing about it is it can be treated from a more holistic standpoint (in addition to the medicines offered by traditional medicine). Although lifestyle changes are important for this to occur there are some other ways to help speed the process up. Below is the plan I use with my patients that helps get to the bottom of their issues so we can detoxify and rebuild the body as fast as possible.
Details on this approach are as follows:
 A Cellular Level Food Sensitivity Test Anyone suffering from IBD absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
A Cellular Level Food Sensitivity Test Anyone suffering from IBD absolutely must get this test done. There could be foods that you are eating on a regular basis that your body does not agree with and are causing you problems. Instead of elimination diets and the guessing game, this test will identify the foods that are causing you problems so we can get you off those foods temporarily, allowing the gut to heal. Once this is accomplished, food sensitivities are eliminated, you can reintroduce these foods back into your diet.
- Traditional allergists run skin and blood tests to determine food allergies. This food sensitivity test goes a level deeper to study the cellular level of the body, the difference between a food allergy and a food sensitivity.
 Intestinal Permeability Test This test will assess your urine to determine if there are microscopic tears “leaky gut” in the small bowel which allow partially digested food particles, viruses, bacteria, and toxins to enter the blood stream. This can lead to inflammation and changes with the gut bacteria that affect your gut health. Leaky gut is the number one cause of gas, bloating, and food allergies / sensitivities. It typically goes untreated because there is no traditional medical test to diagnose it.
Intestinal Permeability Test This test will assess your urine to determine if there are microscopic tears “leaky gut” in the small bowel which allow partially digested food particles, viruses, bacteria, and toxins to enter the blood stream. This can lead to inflammation and changes with the gut bacteria that affect your gut health. Leaky gut is the number one cause of gas, bloating, and food allergies / sensitivities. It typically goes untreated because there is no traditional medical test to diagnose it.
- When leaky gut is diagnosed, with the right treatment plan, it is one of the easiest things to recover from. Healing leaky gut is the most essential component to a healthy digestive system.
 A Microbiome Stool Test - GI disruptors and bacteria imbalance are the number one cause of IBD. If your gut is overrun by bad bacteria, viruses, and pathogens, it’s difficult for the body to be well. This simple stool test will assess the status of pathogens, viruses, parasites, and bacteria that may be contributing to acute and / or chronic digestive and medical symptoms.
A Microbiome Stool Test - GI disruptors and bacteria imbalance are the number one cause of IBD. If your gut is overrun by bad bacteria, viruses, and pathogens, it’s difficult for the body to be well. This simple stool test will assess the status of pathogens, viruses, parasites, and bacteria that may be contributing to acute and / or chronic digestive and medical symptoms.
- Many gastroenterologists order stool studies but they go through traditional labs such as Sonora or Lab Corp. This test is more comprehensive going deeper into the body and returning many more results.
- With this testing we will have a clear picture of the GI Disruptors affecting your health, allowing us to replenish your gut with healthy bacteria to not only get your body working properly but eliminate symptoms and pain.
 Micronutrient Test –This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
Micronutrient Test –This is the most comprehensive micronutrient test available in science today. It determines how well food is being digested, assimilated, and absorbed. It will provide details specific to what vitamins, minerals, and antioxidants you are deficient in.
- This test is the ultimate guide to what foods and supplements you should and shouldn’t be consuming to offset your deficiencies. This test will give you the answer to why you are tired and have low energy. It is your chance to find out if all those supplements you are taking are necessary. Once you know what your cells really need, it becomes clear on how to replenish them.
- Digestive Enzymes - Digestive enzymes help break down our food into smaller, more absorbable units. Your body cannot absorb the food you eat as is, it can only absorb nutrients. Therefore, for your body to benefit from what you eat, proteins need to be broken down into amino acids; fats need to be broken down into fatty acids and cholesterol; and carbohydrates need to be broken down into simple sugars. You rely on digestive enzymes to break down what you eat.
- If you are enzyme deficient, you are not absorbing nutrients from your food, even if the food you are eating is very healthy.
- In addition to not being able to absorb nutrients from what you are eating, enzyme deficiency can also cause many digestive symptoms such as acid reflux, heartburn, indigestion, nausea and vomiting, constipation, and diarrhea.
- At birth we are given a certain potential for manufacturing enzymes in our body, creating an enzyme “reserve.” However, if we do not continually replenish that reserve through proper nutrition, it runs out. With every decade of life our enzyme production depletes by 13%.
 Our Digestive Enzymes are called Everyday Enzymes™. They are what I like to call medical grade enzymes (high potency and no fillers). This is important when taking a supplement, especially a Digestive Enzyme. It is meant to be taken with meals to help you digest your food better. Remember, your GI tract is one long hallow tube from start to finish. If it doesn’t go well in the stomach, it’s probably not going to go well coming out the other end. Digesting your food well is the first step in having good, regular bowel movements and helping your body to absorb much needed vitamins and minerals.
Our Digestive Enzymes are called Everyday Enzymes™. They are what I like to call medical grade enzymes (high potency and no fillers). This is important when taking a supplement, especially a Digestive Enzyme. It is meant to be taken with meals to help you digest your food better. Remember, your GI tract is one long hallow tube from start to finish. If it doesn’t go well in the stomach, it’s probably not going to go well coming out the other end. Digesting your food well is the first step in having good, regular bowel movements and helping your body to absorb much needed vitamins and minerals.
- Probiotics -Your digestive system is home to trillions of microorganisms, creating an ecosystem called the “gut flora.” Probiotics are good bacteria, which are needed to create a balance throughout the body. The body has both good and bad bacteria. Without a healthy balance of good bacteria, symptoms may occur such as diarrhea, constipation, gas, and bloating.
- On a daily basis, we unconsciously consume various microbes that could potentially cause sickness. In a body that has plenty of “good bacteria,” these microbes will pass with no negative effects.
- However, if bad microbes are ingested in a body with an imbalanced gut flora, these microbes will cause sickness. The “bad bacteria” that are constantly in our system, are kept under control by the “good bacteria.”
 Our Probiotics are called Pleasant Probiotics™. These are also medical grade (high potency and no fillers). It contains six strains of bacteria and a lot of each strain; this can’t be said for most probiotics on the market. Our product also has a prebiotic which is food for bacteria. Probiotics are meant to be taken on an empty stomach. We dose ours one in the morning and one at night. Taking a healthy probiotic daily is one of the simplest things you can do, not only for your digestive health but your overall health.
Our Probiotics are called Pleasant Probiotics™. These are also medical grade (high potency and no fillers). It contains six strains of bacteria and a lot of each strain; this can’t be said for most probiotics on the market. Our product also has a prebiotic which is food for bacteria. Probiotics are meant to be taken on an empty stomach. We dose ours one in the morning and one at night. Taking a healthy probiotic daily is one of the simplest things you can do, not only for your digestive health but your overall health. - More than half of our immune system is in the gut wall, so it is vital to keep that part of our body healthy. Many illnesses can be linked back to abnormal gut flora.
- Protease Enzymes / Detoxifying Daily – Proteolytic enzymes, also called protease, break down proteins in the body. If you are familiar with digestive enzymes you know that protease is just one of many enzymes that help break down the food we eat on a daily basis. However, protease enzymes go even further by helping to break down proteins throughout the whole body. The formulation of protease enzymes found in our Delicate Detox™ is designed to work only in the blood (on the whole-body level) instead of just in the stomach. What good do protease enzymes do in the blood; you may ask? Well, just about everything that makes us sick is either a protein or is protected by a protein.
 Bacteria, viruses, yeasts, and fungi are all protected by proteins. In addition, cancer cells are protected by proteins. Food allergens are also proteins. Many food allergies come from us not digesting our food well enough.
Bacteria, viruses, yeasts, and fungi are all protected by proteins. In addition, cancer cells are protected by proteins. Food allergens are also proteins. Many food allergies come from us not digesting our food well enough. - If we don’t have the proper digestive enzymes to break down our food daily and our food enters our small bowel partially digested, large protein molecules can get absorbed into the blood stream. This causes your immune system to kick-in and antibodies are formed with proteins to “protect” the body. Circulating Immune Complexes (CIC’s) are then formed. Basically, this means that your body has now created an immune response “tagged” to something that it shouldn’t. When this happens over and over, the body “stores” these “tags” into its own tissue, because it is now overwhelmed with trying to eliminate them through urination and sweat. This is why the body attacks its own tissue at times, as seen in diseases like lupus, rheumatoid arthritis, and IBD. Supplementing with a proteolytic enzyme can help break down CIC’s, so that they can be passed through urine or sweat easily.
- The blood not only carries oxygen and nutrients throughout the body, it’s also a way for cells and organs to dispose of their garbage and dead material. One way to cleanse the blood is taking a protease enzyme supplement, which can break down things that would otherwise compromise the immune system.
- In addition, these proteolytic enzymes can improve circulation by eating excess fibrin. Fibrin is a strong protein responsible for the development of blood clots. Excess fibrin makes the blood thick, which is a dangerous situation.
- As a result of cleaning out the blood the following can occur; inflammation is reduced, blood flow is optimized, blood clots are prevented, allergies are minimized, arterial plaque is dissolved, headaches are minimized, and cardiovascular health is optimized. Which is why when people start taking the Delicate Detox™ they are able to start fixing more than just their digestive system.
- There are not many supplements on the market that compare to our Delicate Detox™. Not only are they unique, but they are also what I like to call medical grade (high potency and no fillers). This is important when taking a supplement, especially protease enzymes. It is meant to be taken on an empty stomach. I usually take 2 when I wake up and 2 before going to bed.
- Greens -Most people diagnosed with IBD are struggling with fatigue. And if you are struggling with fatigue, you are definitely suffering from vitamin and mineral deficiencies. One of the easiest things you can do to counter that is take a pure vitamin and mineral supplement.
 Our Greens supplement is called Gastro Greens™. These are also medical grade (high potency and no fillers). It contains green food that has been dried and pulverized and put into a capsule. We dose 3 per day; it doesn’t matter when you take them, all 3 at the same time or 1 with every meal.
Our Greens supplement is called Gastro Greens™. These are also medical grade (high potency and no fillers). It contains green food that has been dried and pulverized and put into a capsule. We dose 3 per day; it doesn’t matter when you take them, all 3 at the same time or 1 with every meal. - These are meant to take the place of a standard one-a-day multi-vitamin because your body wants to get vitamins and minerals from real food not synthetic capsules made in a lab.
- I also encourage you to get off gummy vitamins. They may taste good, but they are loaded with sugar / artificial sugar and are doing more damage to the body than good.
- Green food is what builds the body, it’s what builds the blood. If you’re not eating a lot of green this is a great way to supplement it. And if you are eating green, this is a great way to get even more into the body every day. The vegetables we eat today are less nutritious than the vegetables our grandparents ate due to our soil being depleted. Anything you can do to get more vitamins and minerals in the body, the better.
- Increase your daily dose of Gastro Greens™ each day if you are sick or hurt, it will speed up your recovery time.
 Liver Support – although it is important to eat a cleaner diet, slow down on alcohol, nicotine and drugs, it never hurts to add a supplement to your daily routine that is specifically made to help support and repair the liver. Many of our patients have had great success with IBD remission with daily supplementation.
Liver Support – although it is important to eat a cleaner diet, slow down on alcohol, nicotine and drugs, it never hurts to add a supplement to your daily routine that is specifically made to help support and repair the liver. Many of our patients have had great success with IBD remission with daily supplementation.
- Our Liver supplement is called Love Thy Liver™. This formula promotes optimum liver as well as lymphatic system function by encouraging the normal removal of toxic materials and supporting the liver’s normal regeneration sequence.
- It includes a synergistic formulation of herbs (milk thistle and dandelion) and nutrients (N-Acetyl Cysteine) known for their ability to protect the liver, promote hepatic cell regeneration, and support detoxi¬cation.
- This product is the perfect choice to help counter exposure to various forms of environmental toxicity (the air we breathe, alcohol, nicotine, drugs, chemicals in food, drinks, skin products etc.)
- It’s also very effective when used to provide nutritional support before, during, and after a heavy metal detox or other types of aggressive cleanses.
 Alkaline Water – Remember how I stated above, “not all water is created equal”. Alkaline water is what I was referring to. If you are suffering from IBD, drinking more water is important but drinking alkaline water can take your health to the next level. The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
Alkaline Water – Remember how I stated above, “not all water is created equal”. Alkaline water is what I was referring to. If you are suffering from IBD, drinking more water is important but drinking alkaline water can take your health to the next level. The “alkaline” in alkaline water refers to its pH level. A pH level is a number that measures how acidic or alkaline a substance is on an approximate scale of 0 to 14. For example, something with a pH of 1 would be very acidic, and something with a pH of 13 would be very alkaline. Regular drinking water generally has a neutral pH of 7. Alkaline water typically has a pH of 8 or 9.
- Just like a fish tank or a swimming pool, our body needs to maintain a certain pH to stay healthy. If we get really sick and are in the hospital, our pH is monitored because if it drops below a certain amount we can die. When we are healthy, we don’t pay much attention to our pH, but that doesn’t mean it’s not important. On the pH scale, our body is slightly alkaline, so anything you can do to drink and eat more alkaline makes it easier for your body to maintain its alkalinity and in turn work to keep you healthy.
- Your body is a healing vessel, it wants you to be well. Sometimes we just need to help it out a little. Drinking alkaline water is one simple thing you can do to help your body out. It’s especially helpful for people who need to detox the body because it allows more water to absorb into the cells.
 Electrolytes -Electrolytes are critical to our health. They are the pathways our cells use to communicate with each other. Without electrolytes our body is dehydrated. There are so many health symptoms that come from dehydration, aches and pains being one of many.
Electrolytes -Electrolytes are critical to our health. They are the pathways our cells use to communicate with each other. Without electrolytes our body is dehydrated. There are so many health symptoms that come from dehydration, aches and pains being one of many.
- Our Electrolytes are called Super Salts™. They contain the four key electrolyte salts that are made up in the body allowing the body to replenish exactly what it is losing daily. Super Salts™ are meant to be put in water, not on food.
- Our Super Salts™ are different from other electrolyte powders or water additives on the market because they have zero preservatives, sugars, or artificial sugars. This is important because many of those additives can cause digestive issues and toxicity in the body. When you take a supplement like this, the goal is to get well, not cause more issues – the cleaner the product you are consuming, the better.
- We suggest putting one scoop of salts (1 teaspoon) in every 26 – 32-ounce bottle of water you drink. If you cannot do this because it is too salty tasting, start by adding ¼ scoop of salts to 26 – 32 ounces of water and then increase from there once you get used to it. Ideally you want to be drinking about 2 – 3 scoops of salt per day.
 Chop, Chop! Cookbook –eating a cleaner diet is a huge step toward IBD remission. Many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
Chop, Chop! Cookbook –eating a cleaner diet is a huge step toward IBD remission. Many patients ask me what I eat on a day-to-day basis. Tina and I thought it would be helpful to create a cookbook sharing some of our favorite foods. It’s filled with over 70 Gut Recovery & Whole-Body Health Recipes including smoothies, snacks, dips, soups, salads, breakfast, lunch, dinner, and desserts. All healthy and all quickly prepared – we have 4 kids and don’t have time to be in the kitchen, so we try to make it as easy as possible to eat healthy.
- The book is available in English and Spanish.
Act Now – 3 Options to Move in the Right Direction
Depending on your level of commitment and interest in a more holistic approach to your IBD, there are three options to consider:
- Good – Good – if you want to start slow and are not sure if this is for you, at least order our supplements –
Everyday Enzymes, Pleasant Probiotics, Delicate Detox™, Gastro Greens™, Love Thy Liver™ , and Super Salts™. The investment is minimal and it’s not hard to incorporate these supplements into your daily routine to see if they can help. I do encourage you to try this regimen for at least 3 months before you decide it’s not working for you. Doing something for only a few days or even a month is not going to make a huge difference in your body, especially if you’ve been struggling with Crohn’s or Colitis for a long time. - Better – if you are ready to make a more serious commitment to turning around your Crohn’s and Colitis and have some money to invest in yourself,consider ordering our
I Need Everything Starter Kit .It includes three months’ worth of all of our supplements – Everyday Enzymes, Pleasant Probiotics, Delicate Detox™, Gastro Greens™ , Love Thy Liver™ , and Super Salts™ . 
- Best – if you have money to invest in yourself, are suffering from other medical issues and you’re sick and tired of feeling sick and tired consider going all in on our
Digestive Revolution™ Ultimate Plan. This is my 4-Step Proprietary System which is an outcomes and scientific based system that starts at the cellular level. The system delivers 4 main outcomes:- Eliminates digestive issues such as gas, bloating, constipation, diarrhea, and acid reflux.
- Removes pain and inflammation from the body.
- Reduces the need for prescription and over-the-counter medications.
- Increases energy, enhances sleep, and the ability to get to your healthy base weight.

No matter what you decide to do, do something! You get sick and remain sick by accident – you get healthy on purpose!
References
- [1] Crohn’s and Colitis Foundation of America – The Facts about Inflammatory Bowel Disease - https://www.crohnscolitisfoundation.org/sites/default/files/2019-02/Updated%20IBD%20Factbook.pdf
- [2] NIH – Symptoms and Causes of Crohn’s Disease - https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease/symptoms-causes#:~:text=One%20cause%20of%20Crohn's%20disease,to%20symptoms%20of%20Crohn's%20disease.
- [3] New York Presbyterian – Symptoms and Causes of Colitis - https://www.nyp.org/digestive/colitis#:~:text=Researchers%20typically%20attribute%20the%20inflammation,Food%20poisoning
- [4] Mayo Clinic – IBD - https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- [5] Web MD - https://www.webmd.com/ibd-crohns-disease/crohns-disease/5-types-crohns-disease
- [6] Crohn’s and Colitis Foundation - https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/types-of-ulcerative-colitis
- [7] Mayo Clinic – Ulcerative Colitis - https://www.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331
- [8] Chronic Pain – Medication Decisions - https://www.mayoclinic.org/chronic-pain-medication-decisions/art-20360371
- [9] WedMD – Side Effects of UC Meds - https://www.webmd.com/ibd-crohns-disease/ulcerative-colitis/ulcerative-colitis-medications-side-effects
These statements have not been evaluated by the Food and Drug Administration.
These products are not intended to diagnose, treat, cure, or prevent any disease.

Liz Cruz, MD
- Award-winning, board-certified gastroenterologist
- Sought-after leader in solving complex digestive health conditions
- 30+ years of dedicated patient service
- Best-selling author, podcaster and international speaker
Dr. Liz Cruz was named Top Gastroenterologist in 2019. She is a Diplomat of the American Board of Internal Medicine and the American Board of Gastroenterology. Dr. Cruz is a member of the American Gastroenterological Association, American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy. In 2014, she received the Quilly Award from the National Academy of Best-Selling Authors® for her Best-Selling Book “Answering the Call".
